Formulation and Development of Tara Gum-mediated Tablets for Delivery of Anticancer Drugs
1Suresh Gyan Vihar University, Jaipur, Rajasthan, India
2Shree Santkrupa College of Pharmacy, Ghogaon, Satara, Maharashtra, India
*Correspondence to: Pravinkumar Dinkar Lade, Research Scholar, Suresh Gyan Vihar University, Jaipur, Rajasthan, India; Assistant Professor, Shree Santkrupa College of Pharmacy, Ghogaon, Satara, Maharashtra, India. E-mail: pdlade78@gmail.com
Received: June 20 2024; Revised: September 4 2024; Accepted: September 19 2024; Published Online: October 12 2024.
Cite this paper:
Lade PD, Singla N. Formulation and Development of Tara Gum-mediated Tablets for Delivery of Anticancer Drugs. BIO Integration 2024; 5: 1–5.
DOI: 10.15212/bioi-2024-0040. Available at: https://bio-integration.org/
Download citation
© 2024 The Authors. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See https://bio-integration.org/copyright-and-permissions/
Abstract
Background: Natural polysaccharide tara gum (TG) has been investigated for several biological uses. The current study involved the administration of imatinib, an anticancer model medication, via TG.
Methods: Imatinib-modified release tablets were developed using a direct compression method with different concentrations of TG and other excipients. Compressed tablets were evaluated for physicochemical properties.
Result: All formulations had an in vitro disintegration time ranging from 10–23 min. Among the formulations, F6 exhibited excellent extended-release behaviour with 72% release over 12 h. TG tablets were rich in phytoconstituents, including saponins, tannins, phenolics, flavonoids, carbohydrates, proteins, and amino acids.
Conclusion: TG has potential in the drug delivery application of anticancer medications as a rate-retarding polymer.
Keywords
Imatinib, modified release, natural gums, phytochemicals, tara gum.
Introduction
Natural polymers are increasingly favored in the pharmaceutical industry for drug delivery systems due to biocompatibility, biodegradability, and capacity for chemical modification. These materials, including chitosan, alginate, and hyaluronic acid, can be tailored to create drug delivery systems, such as nanoparticles, hydrogels, and micelles [1]. The biocompatible nature of natural polymers reduces the risk of adverse immune reactions, enhancing the safety profile of drug delivery systems [2]. Moreover, the biodegradability of natural polymers ensures degradation into non-toxic byproducts, minimizing the risk of long-term accumulation and associated toxicity [3]. The ability of these polymers to be chemically modified allows for precise control over drug release profiles, which is essential for maintaining therapeutic levels over extended periods, especially in the treatment of chronic conditions [4]. Natural polymers have a critical role in the pharmaceutical industry due to biocompatibility, biodegradability, and ability to be chemically modified. These materials, like chitosan, alginate, and hyaluronic acid, can be tailored to create drug delivery systems, including nanoparticles, hydrogels, and micelles [1]. The biocompatible nature of natural polymers minimizes adverse immune responses and enhances the safety profile of the drug delivery system [2]. The biodegradability of natural polymers ensures break down into non-toxic byproducts, which are easily eliminated from the body, thereby preventing long-term accumulation and associated toxicity [3]. Additionally, the inherent ability of natural polymers to be chemically modified allows drug release profiles to be fine-tuned, ensuring sustained and controlled release of therapeutic agents over extended periods [4]. This feature is particularly advantageous for chronic conditions requiring long-term medication adherence. Excellent mucoadhesive qualities are also exhibited by natural polymers, which increase medication bioavailability by extending the duration of drug residency at the absorption site [5]. Furthermore, structural versatility allows for encapsulation of proteins, peptides, and small molecules, thereby broadening the scope of treatable conditions. Overall, natural polymers are integral to developing advanced drug delivery systems that improve therapeutic efficacy and patient compliance [6].
Tara gum (TG), a natural polysaccharide derived from the seeds of the Caesalpinia spinosa tree, belongs to the galactomannan family. This hydrocolloid is valued for thickening, stabilizing, and gelling properties, which have applications in various industries, including pharmaceuticals [7, 8]. The high molecular weight of TG, which is composed of mannose and galactose units, contributes to exceptional viscosity and gel-forming capabilities, making TG an ideal candidate for rate-retarding applications in drug delivery [9]. The ability of TG to form viscous solutions at low concentrations enhances the bioavailability and therapeutic efficacy of active pharmaceutical ingredients (APIs). Furthermore, the mucoadhesive properties of TG increase the residence time of drugs at the absorption site, which is particularly beneficial for oral and buccal drug delivery systems. The stability of TG across a wide range of pH conditions and compatibility with other polymers and excipients further expand the utility of TG in diverse drug delivery applications [10, 11]. The stability of TG in various pH conditions and compatibility with other polymers and excipients further enhance the application of TG in formulating diverse drug delivery systems. Overall, the natural origin and functional properties of TG make TG a valuable component in modern pharmaceutical formulations [12].
Despite the success of conventional drug delivery systems, there remains significant challenges in the controlled release and bioavailability of anticancer medications. Tyrosine kinase inhibitors (TKIs), such as imatinib, which are widely used in treating gastrointestinal stromal tumors (GISTs) and chronic myeloid leukemia (CML), are limited by rapid drug clearance and the need for frequent dosing and can lead to decreased patient compliance and potential side effects [13]. The potential of TG to overcome these limitations through rate-retarding and mucoadhesive properties makes TG a promising candidate for improving the delivery and efficacy of anticancer medications. However, application of TG in anticancer drug delivery, especially in tablet formulations, remains underexplored. The mechanism of action for TKIs involves blocking the BCR-ABL protein, which promotes cancer cell growth [13]. Imatinib revolutionized CML treatment and significantly improved patient outcomes and survival rates. Natural polysaccharide TG has been investigated for a number of biological uses [14, 15]. In the current study we selected the anticancer agent, imatinib, as a model drug to further explore drug delivery application.
This study aimed to determine the potential of TG as a natural polymer for developing controlled-release tablets of imatinib. By leveraging the unique properties of TG, this study sought to address the challenges of conventional anticancer drug delivery systems, providing a more effective and patient-friendly formulation.
Materials and methods
Materials
The plant material (TG isolate) and other excipients, such as talc, Aerosil®, magnesium stearate, lactose DCL-21, and sodium starch glycolate, were obtained from Vineet Analytical Research Laboratories Pvt Ltd. (Pioma Chemicals, Mumbai, Maharashtra, India).
Formulation of tablets using TG
Tablets containing imatinib were developed using TG extract. Conventional tablets were made with a variable ratio of excipients to TG utilizing the direct compression process. All excipients were well-mixed except magnesium stearate. Following adequate mixing of the extract and other ingredients, Aerosil® and magnesium stearate were added and combined for a further 2–3 min. A rotary punching machine with a 6-mm flat punch was used to crush the tablets [16]. The composition of all formulations is listed in Table 1.
Table 1 Formula Composition of 50-mg Imatinib Tablets
| Sr. No | Ingredients | F1 | F2 | F3 | F4 | F5 | F6 |
|---|---|---|---|---|---|---|---|
| 1 | Imatininb | 50 | 50 | 50 | 50 | 50 | 50 |
| 2 | TG | 100 | 120 | 140 | 160 | 180 | 200 |
| 3 | Talc | 10 | 10 | 10 | 10 | 10 | 10 |
| 4 | Aerosil® | 8 | 8 | 8 | 8 | 8 | 8 |
| 5 | Magnesium stearate | 4 | 4 | 4 | 4 | 4 | 4 |
| 6 | Lactose DCL-21 | 158 | 128 | 98 | 68 | 38 | 8 |
| 7 | Sodium starch glycolate | 50 | 60 | 70 | 80 | 90 | 100 |
| 8 | Total | 380 | 380 | 380 | 380 | 380 | 380 |
All quantities are in mg.
Characterization of tablets [17]
Thickness
Tablet thickness was measured using vernier caliper and recorded.
Weight variation
A sample of 20 tablets was obtained at random from each batch and weighed separately. Twenty tablets were weighed and the average and standard deviation were determined. If no tablet weight deviated from the average weight by more than the percentage shown in Table 1 and no tablet weight deviated by more than twice that percentage, the batch passed the weight variation test.
Hardness
Hardness was measured using a Pfizer hardness tester (Dolphin Pharmacy, Mumbai, Maharashtra, India).
Friability
A Roche friabilator (Testing lab Instruments, Mumbai, Maharashtra, India) was filled with 20 weighted tablets and revolved at 25 rpm for 4 min. The tablets were re-weighed after dedusting and revolutionizing. The friability was calculated using the following equation:
where, %F = % friability
W = Initial weight of the tablet
Wt = tablet weight after revolution.
Disintegration test
Six cylindrical glass tubes were supported by a rigid basket rack assembly in which the tablets were placed. The glass tube dimensions were as follows: length, 77.5±2.5 mm; internal diameter, 21.5 mm; and wall thickness, 2 mm. The assembly was suspended in a 1000-ml beaker in liquid media. The amount of liquid was such that the lowest point of the wire mesh was 25 mm below the liquid surface and 25 mm above the beaker bottom. A temperature of 37°C was kept constant. The average disintegration time was noted.
Content uniformity
The drug content of imatinib tablets was determined by weighing 10 tablets from each formulation and grinding the tablets into a fine powder. After dissolving part of the powder in methanol (20 mg of imatinib), the mixture was filtered through filter paper. After an appropriate dilution, the absorbance at 238 nm was measured using a UV-visible spectrophotometer to determine the amount of imatinib present.
Phytochemical screening
The optimized tablet formulation was used for the initial phytochemical per standard procedures [18].
In vitro dissolution study
The USP type-II dissolving apparatus was utilized for performing dissolution. A paddle and 1000 ml of 0.1N HCl at 37±0.5°C made up the dissolving medium and stirrer running at 50 rpm. One tablet was used in each test. The dissolving liquid was drawn out in increments of 10 ml between 5 and 60 min in advance. An equivalent volume of new media was used to replace the samples that were removed. The samples were subsequently run through a 0.45-μ membrane filter paper and the absorbance at 238 nm was determined. The drug amount was calculated using a calibration curve and recorded as the total quantity of medication dissolved. Three duplicates of the dissolution investigations were completed.
Results and discussion
Development of imatinib tablets containing TG
The extracted TG mucilage was utilized for the development of extended-release tablets with varying concentrations of TG. The tablets were manufactured using a direct compression method. The direct compression technique for tablet formulation is crucial because the direct compression technique simplifies the manufacturing process, reduces production costs, and enhances stability [19]. The direct compression technique eliminates the need for wet granulation, thus avoiding heat and moisture, making the direct compression technique ideal for moisture-sensitive and heat-labile drugs [20]. The developed tablets were characterized for physical parameters, which are presented in Table 2.
Table 2 Physical Properties of Imatinib Tablets
| Batch No. | Weight Variation (mg) | Thickness (mm) | Diameter (mm) | Friability (%) | Hardness (N) | DT (min.) | Drug Content (%) |
|---|---|---|---|---|---|---|---|
| F1 | 385.2±9.48 | 8.5±0.2 | 6.04±0.03 | 0.8 | 5.3±0.9 | 16 | 98.20±1.12 |
| F2 | 382.4±1.52 | 8.4±0.3 | 6.00±0.13 | 0.76 | 4.9±0.4 | 14 | 98.21±1.80 |
| F3 | 381.8±1.62 | 8.5±0.1 | 6.02±0.02 | 0.6 | 4.0±0.6 | 18 | 98.41±1.50 |
| F4 | 384.2±1.26 | 8.4±0.2 | 6.03±0.01 | 0.86 | 4.8±0.5 | 17 | 98.11±1.13 |
| F5 | 380.7±1.64 | 8.4±0.3 | 6.02±0.01 | 0.93 | 4.6±0.3 | 23 | 98.56±0.99 |
| F6 | 383.4±1.38 | 8.5±0.1 | 6.03±0.02 | 0.45 | 4.7±0.8 | 10 | 100.20±1.1 |
A round punch (6 mm in diameter) was used to compress the tablets. The diameter of the compressed tablets ranged from 6.00±0.13 mm to 6.04±0.03 mm, which is acceptable (acceptance criteria, ±2% to ±5% of the punch diameter [5.70–6.30 mm]) given the punch dimensions. Minimal weight variation was observed, ranging from 380.7±1.64–385.2±9.48 mg (acceptance limit, ±7.5% of the tablet weight) due to the excellent flow properties of the granules that ensured complete die filling. The content uniformity was excellent, ranging from 100.20±1.1–98.11±1.13%, meeting the USP limit for uncoated tablets weighing >324 mg, which requires content uniformity within 5%. Tablet hardness ranged from 4.0±0.6–5.3±0.9 N. Friability, assessed using a Roche friabilator, was within the acceptable range of 0.45–0.93% (acceptance criteria, <1%). The thickness of the tablets ranged from 8.4±0.2–8.5±0.2 mm. All formulations had an in vitro disintegration time ranging from 10–23 min.
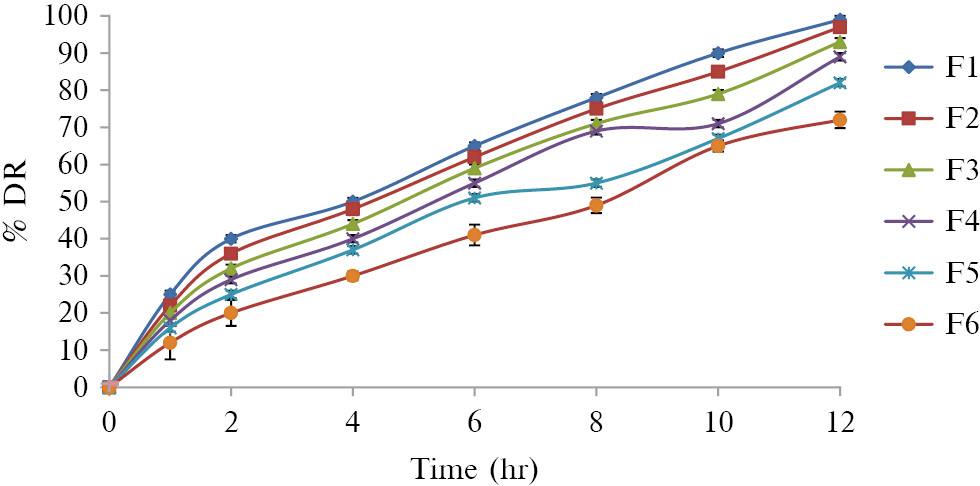
In vitro dissolution study
The comparative dissolution profile is presented in Table 3 and Figure 1. All formulation batches were shown to have extended release behavior. Among the formulations, F6 exhibited excellent extended release behavior with 72% release over 12 h. Table 3 shows the percentage drug release with respect to time for all the formulations.
Table 3 Comparative Drug Release Profile in 0.1N HCl
| Time (hr) | % Drug Release From Formulation |
|||||
|---|---|---|---|---|---|---|
| F1 | F2 | F3 | F4 | F5 | F6 | |
| 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 1 | 25 | 22 | 20 | 18 | 16 | 12 |
| 2 | 40 | 36 | 32 | 29 | 25 | 20 |
| 4 | 50 | 48 | 44 | 40 | 37 | 30 |
| 6 | 65 | 62 | 59 | 55 | 51 | 41 |
| 8 | 78 | 75 | 71 | 69 | 55 | 49 |
| 10 | 90 | 85 | 79 | 71 | 67 | 65 |
| 12 | 99 | 97 | 93 | 89 | 82 | 72 |
Figure 1 Comparative dissolution profile of imatinib tablets in 0.1N HCl.
The ability of cancer therapy tablets to exhibit extended-release behavior is essential because a steady and sustained release of the medication is guaranteed, preserving therapeutic levels in the circulation for a longer amount of time [21]. By reducing the frequency of dose, patient compliance and convenience are enhanced. Sustained release also helps maintain steady-state drug concentrations, reducing the risk of peaks and troughs that can lead to side effects or sub-therapeutic effects. Controlled release enhances the efficacy of treatment, potentially leading to better outcomes in managing cancer [22]. This approach also targets specific timing for drug release, aligning with circadian rhythms for optimal effectiveness.
Phytochemical screening
The results of the phytoconstituents are presented below.
Steroids, alkaloids, fats, and oils were absent in TG mucilage tablets. Other important phytoconstituents, such as saponins, tannins, phenolics, flavonoids, carbohydrates, proteins, and amino acids, were abundantly present (Table 4). The phytochemical screening revealed that TG is rich in phytoconstituents and might be researched as a potential natural remedy for a range of ailments.
Table 4 Phytochemical Test of Different Formulations at Different Time Intervals
| Sr. No. | Plant Constituents | Test/Reagent | TG Tablet |
|---|---|---|---|
| 1 | Steroids | Salkovaski | −− |
| 2 | Alkaloids | Dragendroff’s test | −− |
| Hager’s test | −− | ||
| Mayer’s test | −− | ||
| Wagner’s test | −− | ||
| 3 | Saponins | Foam test | ++ |
| Hemolysis test | ++ | ||
| 4 | Fats and oils | Filter paper test | −− |
| 5 | Tannins and Phenolic | Ferric chloride test | ++ |
| Lead acetate test | ++ | ||
| Potassium dichromate | ++ | ||
| Bromine water | ++ | ||
| 6 | Flavonoids | Shinoda test | ++ |
| Lead acetate test | −− | ||
| 7 | Carbohydrates | Molisch test | ++ |
| Fehling’s test | ++ | ||
| Barfoed’s test | ++ | ||
| 8 | Proteins | Millon’s test | ++ |
| Biuret test | ++ | ||
| 9 | Amino acid test | Ninhydrin test | ++ |
+ve: present; −−ve: absent.
Conclusion
In the current study, TG was shown to be efficiently used as a rate-retarding natural polymer and successfully explored in drug delivery of anticancer agents. All the table parameters were within an acceptable range with excellent modified release properties for a period of 12 h. Moreover, TG tablets are rich in various phytoconstituents, including saponins, tannins, phenolics, flavonoids, carbohydrates, proteins, and amino acids.
Conflict of interest
The authors declare that there are no conflicts of interest.
References
- Idrees H, Zaidi SZ, Sabir A, Khan RU, Zhang X, et al. A review of biodegradable natural polymer-based nanoparticles for drug delivery applications. Nanomaterials (Basel) 2020;10(10):1970. [PMID: 33027891 DOI: 10.3390/nano10101970]
- Kutner N, Kunduru KR, Rizik L, Farah S. Recent advances for improving functionality, biocompatibility, and longevity of implantable medical devices and deliverable drug delivery systems. Adv Funct Mater 2021;31(44):2010929. [DOI: 10.1002/adfm.202010929]
- Huang P, Wang X, Liang X, Yang J, Zhang C, et al. Nano-, micro-, and macroscale drug delivery systems for cancer immunotherapy. Acta Biomater 2019;85:1-26. [PMID: 30579043 DOI: 10.1016/j.actbio.2018.12.028]
- Finbloom JA, Sousa F, Stevens MM, Desai TA. Engineering the drug carrier biointerface to overcome biological barriers to drug delivery. Adv Drug Deliv Rev 2020;167:89-108. [PMID: 32535139 DOI: 10.1016/j.addr.2020.06.007]
- Gómez-Guillén MC, Montero MP. Enhancement of oral bioavailability of natural compounds and probiotics by mucoadhesive tailored biopolymer-based nanoparticles: a review. Food Hydrocoll 2021;118:106772. [DOI: 10.1016/j.foodhyd.2021.106772]
- Lopes CM, Bettencourt C, Rossi A, Buttini F, Barata P. Overview on gastroretentive drug delivery systems for improving drug bioavailability. Int J Pharm 2016;510(1):144-58. [PMID: 27173823 DOI: 10.1016/j.ijpharm.2016.05.016]
- Prajapati VD, Jani GK, Moradiya NG, Randeria NP, Nagar BJ, et al. Galactomannan: a versatile biodegradable seed polysaccharide. Int J Biol Macromol 2013;60:83-92. [PMID: 23707734 DOI: 10.1016/j.ijbiomac.2013.05.017]
- Razavi SM. Introduction to emerging natural hydrocolloids. In: Emerging natural hydrocolloids: rheology and functions. 2019. pp. 1-52.
- Rohilla S, Chawla G, Bhagwat DP, Rohilla A. Natural gum: an option to prepare nanocarriers. Med Theor Hypothesis 2023;6(3):15. [DOI: 10.53388/TMRTH202309015]
- Desai S, Prajapati V, Chandarana C. Chemistry, biological activities, and uses of tara gum. In: Gums, resins and latexes of plant origin: chemistry, biological activities and uses. Cham: Springer International Publishing; 2022. pp. 1-25.
- Mukherjee K, Roy S, Giri TK. Effect of intragranular/extragranular tara gum on sustained gastrointestinal drug delivery from semi-IPN hydrogel matrices. Int J Biol Macromol 2023;253:127176. [DOI: 10.1016/j.ijbiomac.2023.127176]
- Liu F, Chang W, Chen M, Xu F, Ma J, et al. Film-forming properties of guar gum, tara gum and locust bean gum. Food Hydrocoll 2020;98:105007. [DOI: 10.1016/j.foodhyd.2019.03.028]
- Ravegnini G, Sammarini G, Angelini S, Hrelia P. Pharmacogenetics of tyrosine kinase inhibitors in gastrointestinal stromal tumor and chronic myeloid leukemia. Expert Opin Drug Metab Toxicol 2016;12(7):733-42. [PMID: 27149004 DOI: 10.1080/17425255.2016.1184649]
- Din OS, Woll PJ. Treatment of gastrointestinal stromal tumor: focus on imatinib mesylate. Ther Clin Risk Manag 2008;4(1):149-62. [PMID: 18728705 DOI: 10.2147/tcrm.s1526]
- Brummer Y, Cui W, Wang Q. Extraction, purification and physicochemical characterization of fenugreek gum. Food Hydrocoll 2003;17(3):229-36. [10.1016/S0268-005X(02)00054-1]
- Sabale V, Paranjape A, Patel V, Sabale P. Characterization of natural polymers from jackfruit pulp, calendula flowers and tara seeds as mucoadhesive and controlled release components in buccal tablets. Int J Biol Macromol 2017;95:321-30. [PMID: 27889336 DOI: 10.1016/j.ijbiomac.2016.11.078]
- Kompella SD, Cheruvu SH, Bharathi A, Sowjanya K. Research article formulation and in-vitro evaluation of sustained release matrix tablets of losartan potassium using natural gums. J Drug Deliv Res 2013;2:17-33.
- Al-Shamari BB, Al-Ali R, Al-Sahi AA. Preliminary phytochemical evaluation and chemical composition of gum isolated from fenugreek seeds. J Biosci Appl Res 2020;6(3):178-89. [DOI: 10.21608/jbaar.2020.119301]
- Azad MA, Osorio JG, Wang A, Klee DM, Eccles ME, et al. On-demand manufacturing of direct compressible tablets: can formulation be simplified? Pharm Res 2019;36:1-4. [PMID: 31650274 DOI: 10.1007/s11095-019-2716-2]
- Jones-Salkey O, Chu Z, Ingram A, Windows-Yule CR. Reviewing the impact of powder cohesion on continuous direct compression (CDC) performance. Pharmaceutics 2023;15(6):1587. [PMID: 37376036 DOI: 10.3390/pharmaceutics15061587]
- Kaur G, Grewal J, Jyoti K, Jain UK, Chandra R, et al. Oral controlled and sustained drug delivery systems: concepts, advances, preclinical, and clinical status. In: Drug targeting and stimuli sensitive drug delivery systems. William Andrew Publishing; 2018. pp. 567-626.
- Bai X, Smith ZL, Wang Y, Butterworth S, Tirella A. Sustained drug release from smart nanoparticles in cancer therapy: a comprehensive review. Micromachines (Basel) 2022;13(10):1623. [PMID: 36295976 DOI: 10.3390/mi13101623]