Deep Learning Based Two-Dimensional Ultrasound for Follicle Monitoring in Infertility Patients
1Institution of Medical Imaging, University of South China, Hengyang, China
2The Seventh Affiliated Hospital University of South China, Hunan Veterans Administration Hospital, Changsha, China
3Medical UltraSound Computing (MUSIC) Lab, National-Regional Key Technology Engineering Laboratory for Medical Ultrasound, Guangdong Provincial Key Laboratory of Biomedical Measurements and Ultrasound Imaging, School of Biomedical Engineering, Health Science Center, Shenzhen University, Shenzhen, China
4Department of Ultrasound Medicine, The Third Affiliated Hospital of Guangzhou Medical University, Guangzhou, China
aThese authors contributed equally to this work.
*Correspondence: Zhiyi Chen, E-mail: zhiyi_chen@usc.edu.cn
Received: September 19 2022; Revised: October 24 2022; Accepted: January 3 2023; Published Online: January 13 2023
Cite this paper:
Liang X, Zeng F, Li H et al. Deep Learning Based Two-Dimensional Ultrasound for Follicle Monitoring in Infertility Patients. BIO Integration 2023; 4(3): 125–131.
DOI: 10.15212/bioi-2022-0024. Available at: https://bio-integration.org/
Download citation
© 2023 The Authors. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See https://bio-integration.org/copyright-and-permissions/
Abstract
Background: A two-dimensional (2D) ultrasound examination is the primary technique for follicle monitoring, but 2D ultrasound follicle monitoring has significant inter- and intra-observer variability in the measurement of follicle diameter. The aim of this study was to propose a novel deep learning-based automated model for accurate 2D ultrasound follicle monitoring and validate the reliability and repeatability in clinical practice.
Methods: A prospective trial including 300 infertile women undergoing ovulation induction (single follicle cycles) or controlled ovarian hyperstimulation (multiple follicle cycles) was conducted in the reproductive center. After 2D ultrasound image acquisition, the mean diameter of each targeted follicle was measured using an automated model, experts, and a novice. Designating the expert assessment as the gold standard, the reliability and repeatability of the automated model for single and multiple follicle cycles were evaluated using the intraclass correlation coefficient and Bland-Altman plots.
Results: A total of 228 and 1065 follicles from single and multiple follicle cycles, respectively, were included. The accurate recognition rate of follicle boundaries using the automated model was 0.931. The inter-observer variability of follicle mean diameter measurements in single and multiple follicle cycles were 0.970 and 0.984 for the automated model and experts, and 0.965 and 0.978 for a novice and experts, respectively. Bland-Altman plots showed that 95% limits of agreement for follicle diameter measurement between the automated model and experts (−2.02 to 2.39 mm and −0.68 to 1.50 mm) was lower than a novice and experts (−1.69 to 2.74 mm and −0.58 to 1.73 mm) for both single and multiple follicle cycles. The intraclass correlation (ICC) of follicle diameters ≥10 mm calculated by the automated model was significantly higher than follicle diameters <10 mm in multiple follicle cycles (0.834 vs. 0.609). There were no significant differences between the two groups in single follicle cycles (0.967 vs. 0.970).
Conclusion: A deep learning-based automated model provides an accurate and fast approach for novices to improve the reliability and receptivity of 2D ultrasound follicle monitoring, especially in multiple follicle cycles and for follicles with a mean diameter ≥ 10 mm.
Keywords
Follicle monitoring, deep learning, ultrasound, image segmentation, In vitro fertilization.
Significance statement
A 2D ultrasound examination is the primary technique for follicle monitoring, but 2D ultrasound follicle monitoring has significant inter- and intra-observer variability. In this study we proposed a novel deep learning-based automated model for accurate 2D ultrasound follicle monitoring. Our results suggest that the proposed method provides an accurate and fast approach for novices to improve the reliability and receptivity for 2D ultrasound follicle monitoring in clinical practice, especially in multiple follicle cycles.
Introduction
In vitro fertilization and embryo transfer (IVF-ET) is one of the most common assisted reproductive techniques currently utilized, and serial follicle monitoring has important clinical significance during treatment [1, 2]. Serial assessments of follicle diameters have been tested to determine the time for oocyte retrieval during assisted reproductive techniques [3]. In clinical practice, a two-dimensional (2D) transvaginal ultrasound examination is the primary technique used to measure ovarian follicle diameter. Two-dimensional transvaginal ultrasound follicle monitoring allows clinicians to determine the number, diameter, and development of follicles; however, 2D transvaginal ultrasound follicle monitoring is subject to high inter- and intra-observer variability [4, 5]. Less experienced sonographers are at a greater risk of misdiagnosis, which increases the number of false positives [6, 7]. Follicle diameter measurement is highly heterogeneous, thus IVF-ET treatment results can vary [8]. In addition, with the age of infertility onset becoming progressively younger, the workload of sonographers has increased significantly and the excessive workload often leads to measurement errors, missed diagnoses, and other adverse conditions.
Automated and accurate measurements of ovarian follicle diameters are important. Thus, the use of automated ultrasound software to improve the precision of diameter measurements has garnered increased attention. As early as 1997, researchers proposed intelligent algorithms for the automated detection of follicles with a recognition rate of approximately 70% [9]. Then, some studies that focused on the recognition of follicles through enhanced algorithms to improve the follicle recognition rate were reported [10, 11]. In addition, intelligent algorithms were not only used for the automated detection of follicles, but also for estimation of the size of follicles and ovarian classification [12, 13]. With the rapid development of intelligent algorithms, research on automated detection and measurement of follicles are on the rise. These studies showed that intelligent algorithms help in the detection and measurement of follicle development of patients to assist clinicians in making medical decisions. Due to advances technology, an ultrasound-based computer-aided diagnosis system based on ultrasound image analysis techniques has been developed and introduced to commercially-available ultrasound machines [14–16]. Artificial intelligence (AI)-assisted ultrasound software can assess multimodal data and provide objective measurements, which can improve the ultrasound clinical workflow and reduce workload. Currently, the clinical utility of software has been evaluated in some studies of female fertility, such as SonoAVC (GE Healthcare, Zipf, Austria) and Virtual Organ Computer-aided Analysis (GE Healthcare, Zipf, Austria). There is no consensus on the measurement effect of these software algorithms. Time-consuming, complicated, operations and decreased accuracy are still problems which limit the clinical application of software algorithms [17, 18]. In this study, we introduced an automated model based on deep learning for fast and precise 2D ultrasound follicle monitoring, and evaluate the accuracy, repeatability, and reliability in clinical practice.
Materials and methods
Patients
Infertility female patients who underwent ovulation induction or IVF treatment in the reproductive center from January–August 2020 were prospectively recruited. The inclusion criteria were as follows: (i) both ovaries present; and (ii) no severe reproductive or systemic illnesses. The exclusion criteria were as follows: (i) incomplete information or images; and (ii) abnormal ovarian mass > 3 cm in diameter. The patients undergoing ovulation induction, who were considered to undergo single follicle cycles, received 50–100 mg of clomiphene citrate on days 5–9. Women undergoing controlled ovarian hyperstimulation (COH) before IVF, who were considered to undergo multiple follicle cycles, were treated using the long, antagonist, or mini-stimulation protocol. The gonadotropin-releasing hormone (GnRH) antagonist was continued until the day of human chorionic gonadotropin (hCG) administration. This study was conducted in strict accordance with the ethical guidelines of the Declaration of Helsinki. Ethical approval was granted by the local Ethics Committee, and each patient was informed about the aim of the present study and signed an informed consent prior to ultrasound examination.
Ultrasound examinations
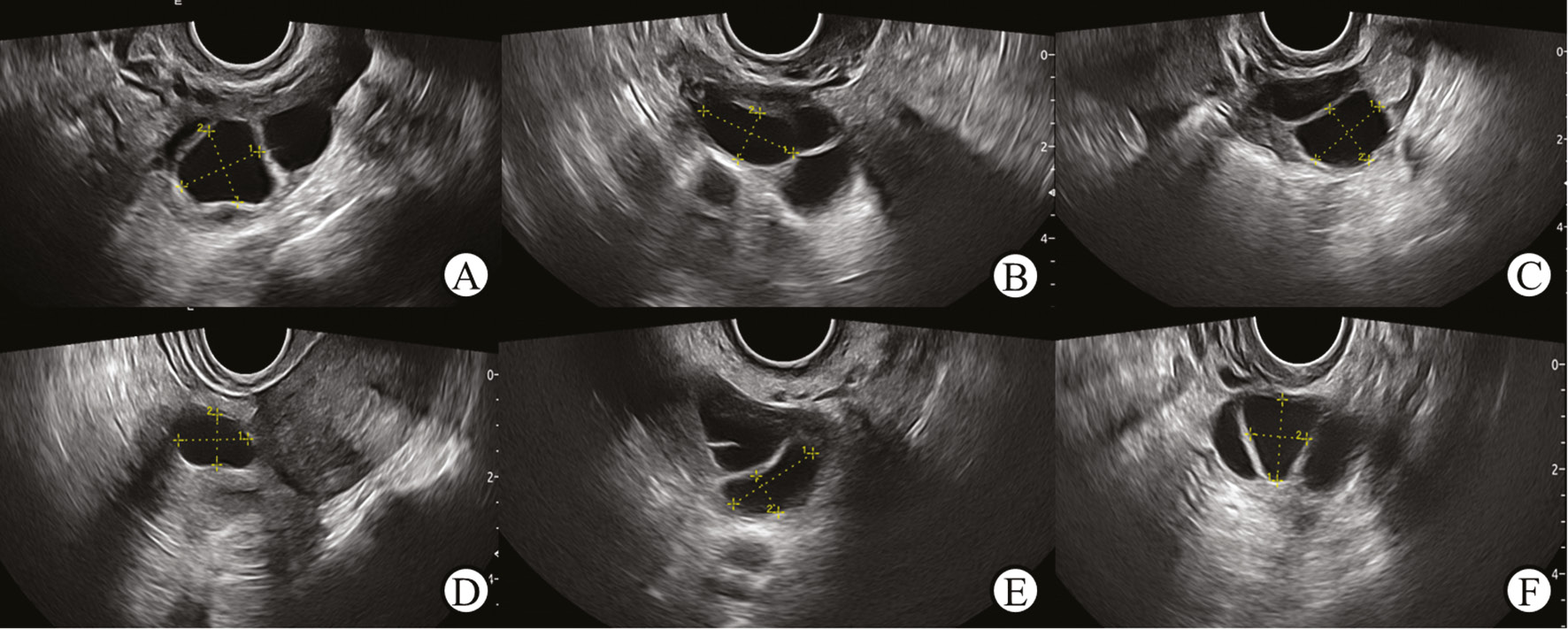
All ultrasound examinations were performed using Acclarix LX9 (Edan Medical, Shenzhen, China) with a 3.0∼10.0 MHz E10-3HQ probe. Examinations and ultrasound image collection were performed by two experts who had 8 years of clinical experience in the evaluation of gynecologic ultrasound data. The boundary of each targeted follicle was clearly visualized during image acquisition. The mean diameter of the follicles was calculated by measuring the vertical lines on the plane of maximum area (Figure 1). During the ultrasound monitoring of single follicle cycles, 5–10 ultrasound images of the leading follicle were collected from each cycle before ovulation, whereas 20–36 follicle ultrasound images were randomly collected from each multiple follicle cycle before oocyte retrieval. The images were exported to an external computer in a JPG file and digital imaging and communications in medicine (DICOM) format.
Figure 1 Mean diameter measurements for different follicle shapes. A. Trapezoid; B. Ellipse; C. Square; D. Semicircle; E. Crescent; F. Triangle.
Statistical analysis
Statistical analysis was performed with SPSS version 25.0 and MedCalc version 20.2. Quantitative data are presented as the mean ± standard deviation. Kappa analysis was used to detect differences between the experts. The follicle border segmentation result evaluated by experts was regarded as the gold standard; only the consistency of the two experts was stable. Bland-Altman plots were used to assess the agreement between automated software, novices, and experts. The maximum allowed difference between methods was set at 2 mm. ICCs and 95% confidence intervals (CIs) were used to assess inter-observer repeatability of ovarian follicle diameter measurements. Repeatability was defined as the consistency between repeated ovarian follicle diameters. A P <0.05 was considered statistically significant.
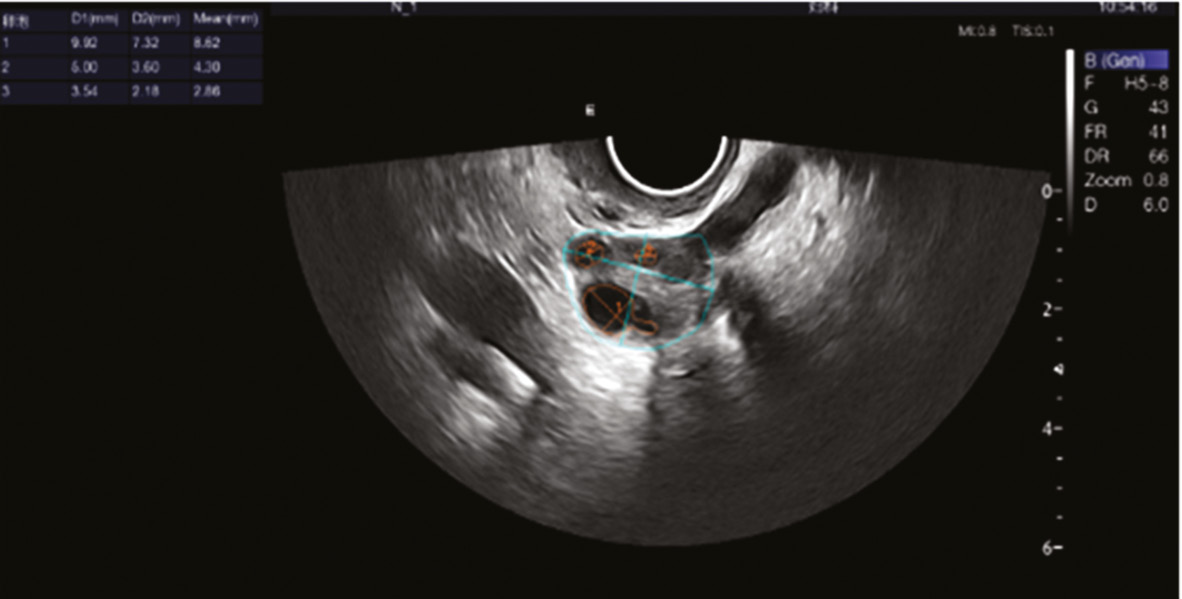
Model establishment and validation
We introduced a cascaded, fine-grained boundary rendering scheme to address the challenges for follicle and ovary segmentation raised by the ambiguous boundaries in ultrasound images. This scheme selectively identified and refined the pixels with high uncertainty around the boundary. The pixels with predicted probabilities of approximately 0.5 were identified as the candidates to be refined. The refinement was then performed by rendering the uncertain predictions based on the fine-grained feature representations, which were re-encoded from the feature activations of Unet. The re-encoding block consisted of two convolutional layers and a lightweight multi-layer perceptron as the prediction head. To determine the context of information and better address the over- and under-segmentation problems, we proposed to further implant the rendering module into a cascaded scheme. Within the cascade, several deep neural networks were stacked stage-by-stage for enhancement of segmentation performance. To further the use of the deep learning model in clinical practice, we packed the algorithm into automated software. Clinical validation was used to evaluate the value of automated software. The software was loaded onto the ultrasound equipment, and automatic follicle mean diameter measurements were performed in each patient (Figure 2). Assessment of accuracy, reliability, and repeatability were performed by two experts with 8 years of ultrasound follicle monitoring experience and 1 novice with 1.5 years of ultrasound follicle monitoring experience.
Figure 2 Operating interface of the automated modal. Blue line: ovarian segmentation and measurement; Orange line: follicular segmentation and measurement.
Results
Patient characteristics
Fifty-eight patients undergoing multiple follicle cycles were excluded from the study; 40 patients have incomplete information or images and 18 patients had cysts or abnormal ovarian masses > 3 cm in diameter during monitoring. Three hundred infertility patients, including 130 undergoing single follicle cycles and 170 undergoing multiple follicle cycles, who agreed to participate in this study. In the final dataset, there were 228 follicle samples in the single follicle cycle group and 1065 follicle samples in the multiple follicle cycle group. Table 1 shows the baseline characteristics of the two groups. There were no significant differences in age, weight, height, and body mass index between the two groups (P > 0.05).
Table 1 Baseline Characteristics of the Patients in Single and Multiple Follicle Cycles
| Characteristics | Multiple Follicle Cycles | Single Follicle Cycles | P Value |
|---|---|---|---|
| Age (year) | 31.3 ± 4.4 | 32.2 ± 5.1 | 0.236 |
| Weight (kg) | 54.1 ± 7.5 | 55.4 ± 9.6 | 0.336 |
| Height (cm) | 157.8 ± 4.7 | 158.0 ± 5.7 | 0.805 |
| BMI (kg/m2) | 21.7 ± 2.8 | 22.2 ± 3.7 | 0.340 |
Values were presented as the mean ± standard deviation. BMI: body mass index. P < 0.05 was considered a statistically significant difference.
Gold standard and model performance
Kappa analysis showed good consistency between the two experts in assessment of follicle border segmentation with a kappa value of 0.790. The accuracy of follicle boundary recognition by the automated model reached 0.931. The reliability of follicle diameter measurements estimated by calculation of the ICC is shown in Table 2. Compared with the novice, the automated model had a higher ICC in mean diameter measurements during single and multiple follicle cycles. According to the 95% limits of agreement, there were no significant differences between the ICCs.
Table 2 Reliability of Follicle Mean Diameter Measured by a Novice and Automated Model in Single and Multiple Follicle Cycles
| Multiple Follicle Cycle | Single Follicle Cycle | |||||
|---|---|---|---|---|---|---|
| ICC | 95% CI | P Value | ICC | 95% CI | P Value | |
| Automated model vs. expert | 0.984 | 0.945–0.993 | <0.001 | 0.970 | 0.961–0.977 | <0.001 |
| Novice vs. expert | 0.963 | 0.896–0.981 | <0.001 | 0.965 | 0.937–0.978 | <0.001 |
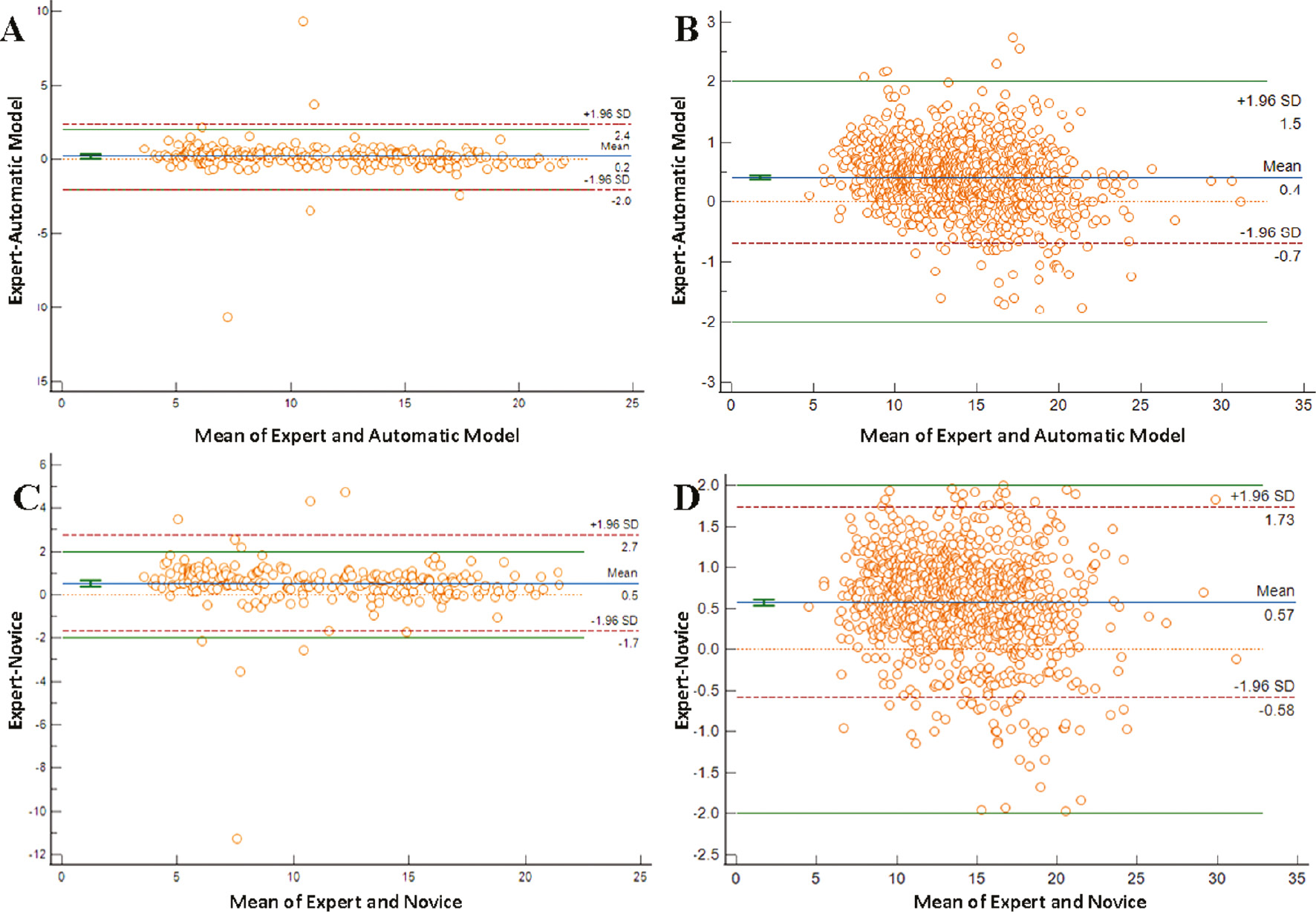
There was no inter- or intra-observer variation for the automated model because the model always outputs the same segmentation result. Bland-Altman plots were used to estimate the repeatability of mean follicle diameter measurements obtained by the automated model, the novice, and experts (Figure 3). The 95% limits of agreement between the automated model and experts (−2.02 to 2.39 mm) was lower than the novice (−1.69 to 2.74 mm) in single follicle cycles. The mean difference values were 0.19 mm and 0.52 mm, respectively. The 95% limits of agreement between the automated modal and experts (−0.68 to 1.50 mm) was lower than the novice and experts (−0.58 to 1.73 mm) in multiple follicle cycles, and the mean difference values were 0.41 mm and 0.57 mm for the automated model and novice, respectively.
Figure 3 Bland-Altman plots for assessment of repeatability in mean diameter measurements. Plots represent the difference between observers’ measurements and mean measurements. The top and bottom lines show the 95% limits of agreement; the middle line shows the mean difference. A and C. single follicle cycles; B and D. multiple follicle cycles.
The criterion for a higher fertilization rate was a mean follicle diameter > 10 mm. In this study, reliability of follicular mean diameter (measured by automated model) greater than or less than 10mm estimated by calculation of the ICC, were 0.967 and 0.834 in single follicular cycles, 0.970 and 0.609 in multiple follicular cycles, respectively (Table 3). ICC value of follicular diameter ≥10 mm calculated by automated model was significantly higher than measurement of follicular diameter <10 mm in multiple follicular cycles. In single follicular cycles, there were no significant differences between the two groups.
Table 3 Reliability of a Follicle Mean Diameter Greater than or Less than 10 mm Estimated by an Automated Model in Single and Multiple Follicle Cycles
| Multiple Follicle Cycle | Single Follicle Cycle | |||||
|---|---|---|---|---|---|---|
| ICC | 95% | P Value | ICC | 95% | P Value | |
| Follicle diameter ≥10 mm | 0.970 | 0.829–0.998 | <0.001 | 0.967 | 0.796–0.988 | <0.001 |
| Follicle diameter <10 mm | 0.609 | 0.352–0.754 | <0.001 | 0.834 | 0.114–0.946 | <0.001 |
Discussion
Ultrasound is an essential and common approach to monitor the development of follicles in the treatment of infertility. Given the significant time required for the measurement of ovarian follicle diameter and variability between different clinicians, AI-assisted technology for monitoring follicles is necessary [19]. In this study we have introduced and validated a novel deep learning-based automated model for fast and accurate segmentation of follicles on 2D ultrasound images. We showed that this automated model improved follicle boundary recognition and achieved higher repeatability and reliability, especially in multiple follicle cycles of patients undergoing COH treatment before IVF.
Currently, measurement of the mean follicle diameter on 2D ultrasound images remains the preferred method to assess follicle size [5]. This method still faces the problem of insufficient standardization; thus, there are significant differences between follicle diameter measurements [20]. Earlier studies constructed models to recognize and measure the follicle [21] that are less time-consuming than manual measurement, especially for irregularly-shaped follicles [22]. One challenge in AI-assisted ultrasound follicle monitoring is to achieve better clinical applicability. Although previous studies have improved the efficiency of follicle recognition and measurement by enhancing existing algorithms or applying new algorithms, the majority of these methods are still in preclinical studies [23]. In our previous study, we proposed a deep learning-based algorithm of CR-Unet for follicle segmentation in which the dice similarity coefficients (DSCs) reached 0.858 [24]. In the present study the results of ICC and Bland-Altman analyses indicated that the variation between the automated model and expert measurements was less than the variation between the novice and expert measurements. The automated model provides a potential approach to improve the accuracy of follicle monitoring, especially for novices and areas lacking medical resources. Our findings are similar to the previous studies [25, 26]. This is the first study to validate a deep learning-based follicle monitoring model performed on 2D ultrasound equipment in clinical practice.
One of the common problems of AI-assisted algorithms is the clinical application efficiency is lower than the laboratory efficiency. Because industrialization is the final goal, the integration among multiple domains and industries is of great significance [27]. In this prospective pilot study, we determined whether an automated model based on a deep learning algorithm could be used to fulfill the clinical demand. This study showed that automated software has achieved a high rate (> 0.90) on the boundary recognition of follicles. We reviewed the dataset and showed that the boundary recognition of 31 multiple and 3 single cycles were incorrect using the automated model. The main reason for this finding was poor image quality, in which the boundaries of the follicles were not clearly recognized.
In studies addressing the impact of follicle monitoring on fertility outcome, it was reported that the fertilization rate increases when the follicular diameter is > 10 mm, and this criterion is also regarded as predicting mature oocytes in ultrasound follicle monitoring [28]. In the current study we drew the follicle samples in two groups based on a mean follicle diameter greater than or less than 10 mm, and further estimated the reliability of measurement obtained by the automated model in both single and multiple follicle cycles. Interestingly, we found that the automated model was conducive to follicle diameter measurement which was ≥ 10 mm. The accurate measurement rate of follicles in multiple follicle cycles was higher than single follicle cycles because the boundary of the follicle diameter ≥ 10 mm is more distinct. It was noted that automated software had inferior performance in follicle diameters < 10 mm in multiple follicle cycles. Follicle overcrowding can cause follicle compression and elongation in one plane, and errors in the measurement of diameters will be exacerbated because of confusion and subjectivity of 2D diameter measurements of follicles in multiple follicle development during COH cycles [29]. In the early stage of follicle development in multiple follicle cycles the emphasis of an AI-assisted model of ultrasound follicle monitoring should be follicle counting, while during the late stage of follicle development, it should be the precise segmentation of follicles ≥ 10 mm.
There were some limitations in our study. The model was verified in a single center, rather than in a multi-center setting. In addition, the image quality was not quantitatively evaluated. Because the automated model was proved to be more applicable to follicles ≥ 10 mm, the performance of deep learning-based segmentation in small follicle tracking and counting was not considered. Continuous improvement of the algorithm will be performed in our corollary studies.
Conclusion
An automated model for 2D ultrasound follicle monitoring, which avoids inter- or intra-observer variation, provides a reliable technique for the novice to improve monitoring accuracy, feasibility, and repeatability, especially in multiple follicle cycles. The automated model for 2D ultrasound follicle monitoring belongs to a class of automated systems that may be useful for ensuring consistency of repeated ovarian follicle diameter measurements, standardize measurement criteria for large cohort studies, and improve the quality of data collection.
Declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of the Third Affiliated Hospital of Guangzhou Medical University (No. 2018-13), and all patients gave written informed consent.
Competing interests
The authors declare that they have no competing interests.
Funding
This work was supported by the Clinical Research 4310 Program of the First Affiliated Hospital of The University of South China (4310-2021-K06) and National Natural Science Foundation of China (82102054).
Authors’ contributions
ZF and LX were responsible for manuscript preparation, concept, and design of the study; LH and ND were responsible for experimental studies and data analysis; and LY, LY, and CK were responsible for data acquisition, manuscript review, and statistical analysis. CZ is responsible for the final approval of the proofs and the integrity of the work.
Acknowledgements
Not applicable
Abbreviations
| 2D | Two-dimensional |
| COH | Controlled ovarian hyperstimulation |
| IVF-ET | In vitro fertilization and embryo transfer |
| AI | Artificial intelligence |
| GnRH | gonadotropin-releasing hormone |
| hCG | Human chorionic gonadotropin |
| DICOM | digital imaging and communications in medicine |
| ICC | Intraclass correlation coefficient |
| CI | Confidence interval |
References
- Sunderam S, Kissin DM, Crawford SB, Folger SG, Jamieson DJ, et al. Assisted reproductive technology surveillance – United States, 2014. MMWR Surveill Summ 2017;66:1-24. [PMID: 28182605 DOI: 10.15585/mmwr.ss6606a1]
- Chen Y, Nisenblat V, Yang P, Yang P, Zhang X, et al. Reproductive outcomes in women with unicornuate uterus undergoing in vitro fertilization: a nested case-control retrospective study. Reprod Biol Endocrinol 2018;16:64. [PMID: 29980195 DOI: 10.1186/s12958-018-0382-6]
- Klenov VE, Van Voorhis BJ. Ultrasound in infertility treatments. Clin Obstet Gynecol 2017;60:108-20. [PMID: 28059846 DOI: 10.1097/GRF.0000000000000263]
- Barczyński M, Stopa-Barczyńska M, Wojtczak B, Czarniecka A, Konture A. Clinical validation of S-Detect™ mode in semi-automated ultrasound classification of thyroid lesions in surgical office. Gland Surg 2020;9(Suppl 2):S77-85. [PMID: 32175248 DOI: 10.21037/gs.2019.12.23]
- Coelho Neto MA, Ludwin A, Borrell A, Benacerraf B, Dewailly D, et al. Counting ovarian antral follicles by ultrasound: a practical guide. Ultrasound Obstet Gynecol 2018;51:10-20. [PMID: 29080259 DOI: 10.1002/uog.18945]
- Skaane P, Engedal K, Skjennald A. Interobserver variation in the interpretation of breast imaging. Comparison of mammography, ultrasonography, and both combined in the interpretation of palpable noncalcified breast masses. Acta Radiol 1997;38:497-502. [PMID: 9240666 DOI: 10.1080/02841859709174375]
- Baker JA, Kornguth PJ, Soo MS, Walsh R, Mengoni P. Sonography of solid breast lesions: observer variability of lesion description and assessment. AJR Am J Roentgenol 1999;172:1621-5. [PMID: 10350302 DOI: 10.2214/ajr.172.6.10350302]
- Murtinger M, Zech MH, Spitzer D, Zech NH. Outpatient follicle monitoring: a plea for standardization in ultrasound based follicle monitoring and data transfer. J Reprod Infertil 2014;15:105-8. [PMID: 24918083]
- Potocnik B, Zazula D, Korze D. Automated computer-assisted detection of follicles in ultrasound images of ovary. J Med Syst 1997;21:445-57. [PMID: 9555630 DOI: 10.1023/a:1022832515369]
- Potocnik B, Zazula D. Automated ovarian follicle segmentation using region growing, In: International Workshop on Image & Signal Processing & Analysis. IEEE; 2000.
- Hiremath P, Tegnoor JR. Automatic detection of follicles in ultrasound images of ovaries using edge-based method. International Journal of Computer Applications 2010;2:120-5.
- Chen T, Zhang W, Good S, Zhou KS, Comaniciu D. Automatic ovarian follicle quantification from 3D ultrasound data using global/local context with database guided segmentation. IEEE International Conference on Computer Vision. IEEE; 2009.
- Kiruthika V, Sathiya S, Ramya MM. Automatic texture and intensity based ovarian classification. J Med Eng Technol 2018;42:604-16. [PMID: 30932717 DOI: 10.1080/03091902.2019.1588407]
- Kim HL, Ha EJ, Han M. Real-world performance of computer-aided diagnosis system for thyroid nodules using ultrasonography. Ultrasound Med Biol 2019;45:2672-8. [PMID: 31262524 DOI: 10.1016/j.ultrasmedbio.2019.05.032]
- Choi YJ, Baek JH, Park HS, Shim WH, Kim TY, et al. Computer-aided diagnosis system using artificial intelligence for the diagnosis and characterization of thyroid nodules on ultrasound: initial clinical assessment. Thyroid 2017;27:546-52. [PMID: 28071987 DOI: 10.1089/thy.2016.0372]
- Cho E, Kim EK, Song MK, Yoon JH. Application of computer-aided diagnosis on breast ultrasonography: evaluation of diagnostic performances and agreement of radiologists according to different levels of experience. J Ultrasound Med 2018;37:209-16. [PMID: 28762552 DOI: 10.1002/jum.14332]
- Wertheimer A, Nagar R, Oron G, Meizner I, Fisch B, et al. Fertility treatment outcomes after follicle tracking with standard 2-dimensional sonography versus 3-dimensional sonography-based automated volume count: prospective study. J Ultrasound Med 2018;37:859-66. [PMID: 28960452 DOI: 10.1002/jum.14421]
- Singh N, Usha BR, Malik N, Malhotra N, Pant S, et al. Three-dimensional sonography-based automated volume calculation (SonoAVC) versus two-dimensional manual follicular tracking in in vitro fertilization. Int J Gynaecol Obstet 2015;131:166-9. [PMID: 26341173 DOI: 10.1016/j.ijgo.2015.04.045]
- Niederberger C, Pellicer A, Cohen J, Gardner DK, Palermo GD, et al. Forty years of IVF. Fertil Steril 2018;110:185-324.e5. [PMID: 30053940 DOI: 10.1016/j.fertnstert.2018.06.005]
- Mascarenhas MN, Flaxman SR, Boerma T, Vanderpoel S, Stevens GA. National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med 2012;9:e1001356. [PMID: 23271957 DOI: 10.1371/journal.pmed.1001356]
- Hiremath PS, Tegnoor JR. Recognition of follicles in ultrasound images of ovaries using geometric features. IEEE; 2009. pp. 1-8.
- Rodriguez A, Guillén JJ, López MJ, Vassena R, Coll O, et al. Learning curves in 3-dimensional sonographic follicle monitoring during controlled ovarian stimulation. J Ultrasound Med 2014;33:649-55. [PMID: 24658944 DOI: 10.7863/ultra.33.4.649]
- Liu J, Chen H. Automatic detection of follicle in ultrasound images of cattle ovarian using MCL method. 2016 IEEE International Conference on Systems, Man, and Cybernetics (SMC). IEEE; 2016.
- Li H, Fang J, Liu S, Liang X, Yang X, et al. CR-Unet: a composite network for ovary and follicle segmentation in ultrasound images. IEEE J Biomed Health Inform 2020;24:974-83. [PMID: 31603808 DOI: 10.1109/JBHI.2019.2946092]
- Liang X, Fang J, Li H, Yang X, Ni D, et al. CR-Unet-based ultrasonic follicle monitoring to reduce diameter variability and generate area automatically as a novel biomarker for follicular maturity. Ultrasound Med Biol 2020;46:3125-34. [PMID: 32839052 DOI: 10.1016/j.ultrasmedbio.2020.07.020]
- Akkus Z, Cai J, Arunnit B, Zeinoddini A, Weston A, Philbrick K, et al. A survey of deep-learning applications in ultrasound: artificial intelligence-powered ultrasound for improving clinical workflow. J Am Coll Radiol 2019;16(9 Pt B):1318-28. [PMID: 31492410 DOI: 10.1016/j.jacr.2019.06.004]
- Saw P, Jiang S. The significance of interdisciplinary integration in academic research and application. BIO Integ 2020;1:2-5. [DOI: 10.15212/bioi-2020-0005]
- Penzias AS, Emmi AM, Dubey AK, Layman LC, DeCherney AH, et al. Ultrasound prediction of follicle volume: is the mean diameter reflective? Fertil Steril 1994;62:1274-6. [PMID: 7957999]
- Re C, Mignini Renzini M, Rodriguez A, Dal Canto M, Buccheri M, et al. From a circle to a sphere: the ultrasound imaging of ovarian follicle with 2D and 3D technology. Gynecol Endocrinol 2019;35:184-9. [PMID: 30394144 DOI: 10.1080/09513590.2018.1522297]