Nanofibers for Drug Delivery: Design and Fabrication Strategies
1Pharmaceutics, St. John Institute of Pharmacy and Research, Palghar, India
*Correspondence to: Aarati Anil Budar, St. John Institute of Pharmacy and Research, Vevoor, Manor Road, Palghar (E), District Palghar, Palghar, Maharashtra 401404, India. Mobile: 7208345358, E-mail: aaratibudar2000@gmail.com
Received: May 14 2024; Revised: May 27 2024; Accepted: July 4 2024; Published Online: August 1 2024
Cite this paper:
Kalayil N, Budar AA, Dave RK. Nanofibers for Drug Delivery: Design and Fabrication Strategies. BIO Integration 2024; 5: 1–18.
DOI: 10.15212/bioi-2024-0023. Available at: https://bio-integration.org/
Download citation
© 2024 The Authors. This is an open access article distributed under the terms of the Creative Commons Attribution License (https://creativecommons.org/licenses/by/4.0/). See https://bio-integration.org/copyright-and-permissions/
Abstract
Nanotechnology is an emerging field with substantial scientific and economic potential globally. Researchers are increasingly focusing on creating nanomaterials for diverse applications. This review explores the potential of drug-loaded nanofibers for drug delivery and describes their production methods, including centrifugal jet spinning, plasma-induced synthesis, solution blow spinning (SBS), pressure spinning, and electrospinning. Nanofibers, owing to their extensive surface area relative to their volume, are believed to enhance interactions with target substances and therefore are valuable in numerous applications. This review provides a thorough exploration of fabrication techniques, encompassing fundamental concepts, methods, and material aspects. Furthermore, it provides perspectives on the variables affecting the production and application of nanofibers, such as electrospinning parameters (including electric field intensity, needle size, flow rate, and distance between the needle and collector), solution characteristics (such as polymer concentration, solvent type, conductivity, and viscosity), and environmental factors (such as temperature and humidity). Additionally, an extensive compilation of patents related to nanofiber-based drug delivery systems is presented, showcasing innovations and advancements in the field. The review also examines current clinical trials involving nanofiber technologies, providing insights into their therapeutic potential and translational prospects. This review is aimed at presenting an overview of nanofiber drug delivery systems, and identifying future opportunities and challenges in their development and application.
Keywords
Applications, controlled release, drug delivery system, electrospinning, electrospun nanofibers, fabrication, kinetics, materials for nanofibers, nanofibers, targeted drug delivery.
Introduction
Various drug delivery systems have been documented for administration via enteral routes, including granules, tablets, and capsules, as well as via parenteral routes, such as intravenous, intra-arterial, intramuscular, and subcutaneous delivery. These drug delivery systems have several disadvantages, including the possibility of first-pass metabolism, which can decrease the drug’s bioavailability, and the potential for discomfort or pain during administration [1]. To address the constraints of conventional immediate-release formulations, a range of novel drug delivery systems have been created, such as microspheres, microsponges, nanoparticles, nanofibers, and hydrogels [2]. Nanofibers are extremely thin fibers, between 1 and 1000 nanometers in diameter, generated from polymers. Through use of polymeric fibers and implementation of controlled-release administration routes, drugs can be applied once or twice daily, thus improving patient adherence and avoiding toxic plasma peak concentrations that can arise from frequent administration of immediate-release formulations [1]. Small nanofibers offer advantages including excellent stability, targeted delivery, high drug-loading capacity, high surface area, diminished toxicity, improved mechanical properties, and suitability for delivery of thermo-sensitive drugs [3]. Various techniques can be used for the preparation of nanofibers, such as emulsion spinning, force spinning, melt spinning, and electrospinning [4]. The purpose of this review is to summarize various techniques used for fabrication, and factors influencing the electrospinning process, and to highlight the wide range of applications of nanofibers.
Nanofiber fabrication techniques
Numerous methods have been effectively used for the production of nanofibers, including the self-assembly method, template synthesis, melt-blown method, electrostatic spinning method, direct stretching method, wet spinning method, plasma-induced synthesis, centrifugal jet spinning method, solution blowing spinning, pressurized spinning, and many others. Electrospinning, plasma-induced synthesis, pressure spinning, centrifugal jet spinning, and solution blow spinning are the most common methods used for the fabrication of nanofibers [2]. Table 1 shows various techniques for the fabrication of nanofibers, along with their drawbacks.
Table 1 Nanofiber Fabrication Methods and their Drawbacks
| Technique | Drawbacks |
|---|---|
| Melt-blown method | Limited to thermoplastic polymers |
| Template synthesis | Cannot produce continuous fibers; removing the nanofibers from the template is complicated |
| Direct stretching method | Manufacturing fibers with a diameter below 100 nm poses challenges; slow production process |
| Self-assembly | Materials used should be amphiphilic and are costly to produce |
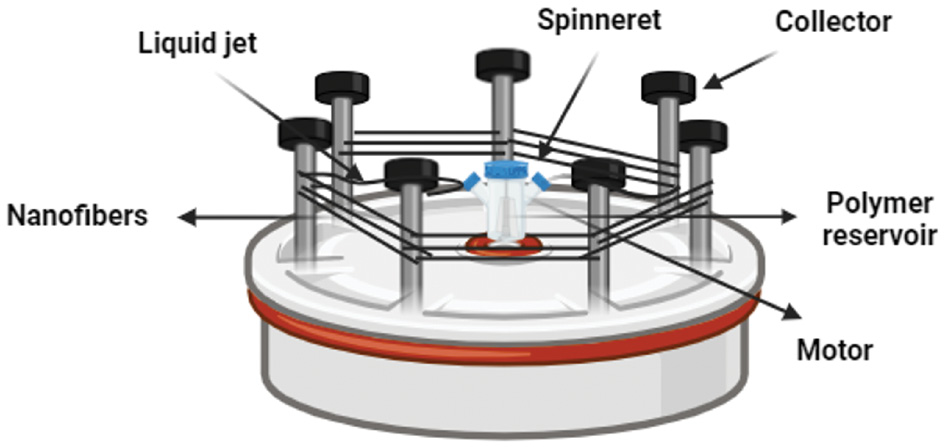
Centrifugal jet spinning
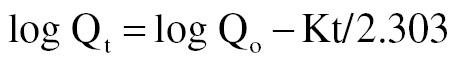
Centrifugal spinning, alternatively termed rotary jet spinning or force spinning, uses centrifugal force to overcome the surface tension of a polymer solution, thus producing fibers spanning from microns to nanometers in diameter. The centrifugal spinning apparatus comprises several components, including a motor, a shaft, a spinneret, and a collector. To initiate the production of nanofibers, the process commences by injecting polymer solution into the spinneret and subsequently subjecting it to rapid rotation [5]. The spinning head holding the polymer solution or melt experiences a surge in centrifugal force as its rotational speed increases, and ultimately exceeds the counteracting force of surface tension. Consequently, a liquid jet is ejected from the nozzle tip, experiences elongation, and is laid down on the collector as nanofibers, with solvent evaporation occurring throughout the stretching process [2]. Figure 1 illustrates the setup of centrifugal jet spinning. This method is ideal for commercial production, because it is more efficient than other techniques and does not require high pressure [5]. The primary limitation of this method is that both the quality of the fibers and the rate of production are markedly affected by the properties of the materials and the design of the spinneret [2]. Unlike traditional electrospinning, forcespinning uses centrifugal force instead of an electric field, thus overcoming the limitations associated with electrospinning, such as high production costs, conductivity issues, low productivity, and high electric field requirements [5].
Figure 1 Centrifugal jet spinning setup.
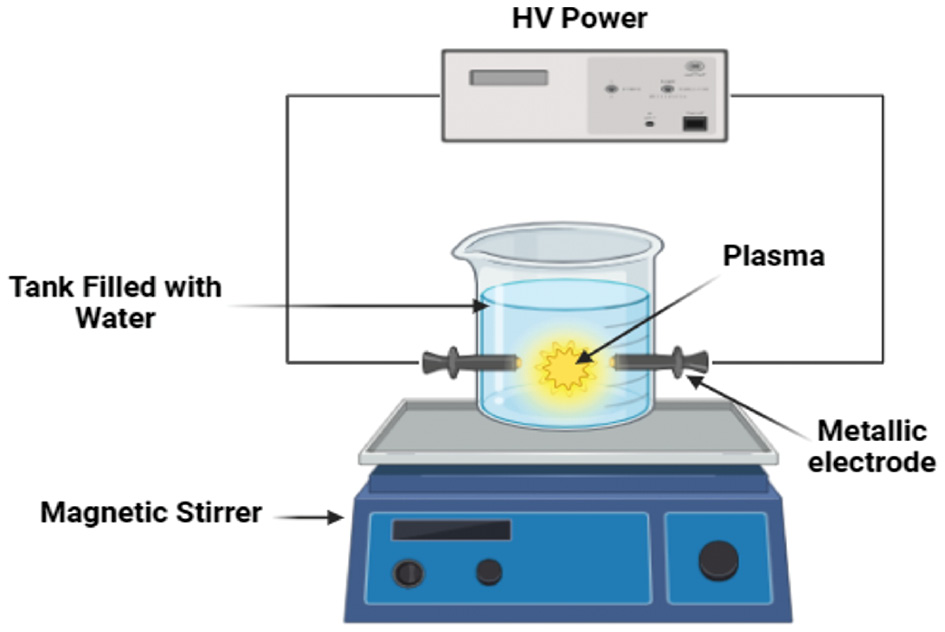
Plasma-induced synthesis
Creating nanofibers through plasma-induced synthesis involves five key stages: (1) radicals forcefully striking the electrode surface, (2) deposition of atomic vapor, (3) plasma expansion, (4) solution medium condensation, and (5) nanofiber growth through an in situ reaction with oxygen [6]. Figure 2 illustrates the setup for plasma-induced synthesis of nanofibers. Electrical energy is used to generate plasma, thereby facilitating the gradual enlargement of precursor atoms into fiber-like structures. To generate plasma in the solution, the precursor material is used to create the electrode, which is submerged in an electrolyte solution and exposed to an electric current. As the plasma expands, and the discharge time increases, atoms coalesce into clusters, which are subsequently oxidized and transformed into fibers [2].
Figure 2 Plasma-induced synthesis of nanofibers.
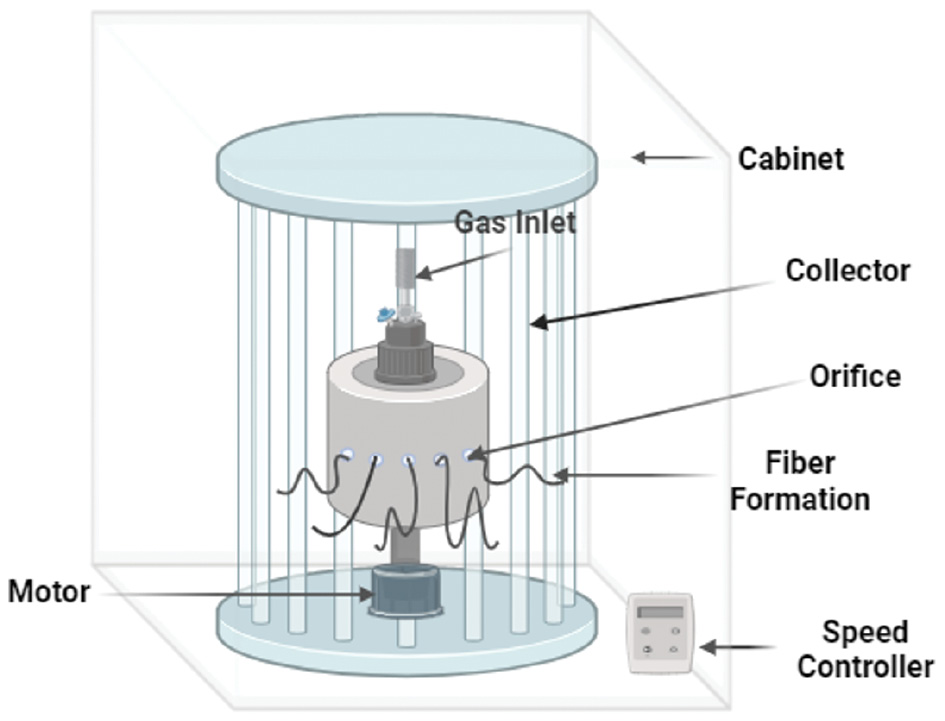
Pressure spinning
Mahalingam and Edirisinghe developed a new process called pressurized gyration (PG), also called pressure spinning, which combines centrifugal spinning and solution blowing to create consistent nanofibers with diameters ranging from 60 to 1000 nanometers. The PG system is composed of a rotating aluminum container with several small openings measuring 0.5 millimeters in circumference [7]. The size of the vessel and orifices, as well as the number of orifices, can be adjusted as necessary. The vessel is equipped with a high-speed motor at one end, capable of reaching speeds as high as 36,000 rpm [8]. At the top of the vessel, a link to a compressed gas cylinder allows for the generation of pressures reaching 0.3 megapascals (MPa) [7]. The high-speed spinning of the vessel creates a polymer stream, which is then drawn out into fibers via an opening. Injecting gas into the vessel can enhance this stretching process. An aluminum foil collector is placed around the spinning vessel to gather the polymer fibers [8]. The PG process involves three primary stages of fiber formation. Figure 3 depicts the setup for pressurized gyration. First, a polymer stream is ejected from the vessel’s opening and starts to elongate. Second, rapid solvent evaporation occurs, causing the fibers to become even thinner. Ultimately, the fibers solidify through evaporation, thus resulting in the creation of delicate and slender fibers. Fiber formation through this method is caused by Rayleigh-Taylor instability, which disturbs the polymer solution jet as it exits the orifice of the PG vessel [7].
Figure 3 Pressurized gyration method of nanofiber preparation.
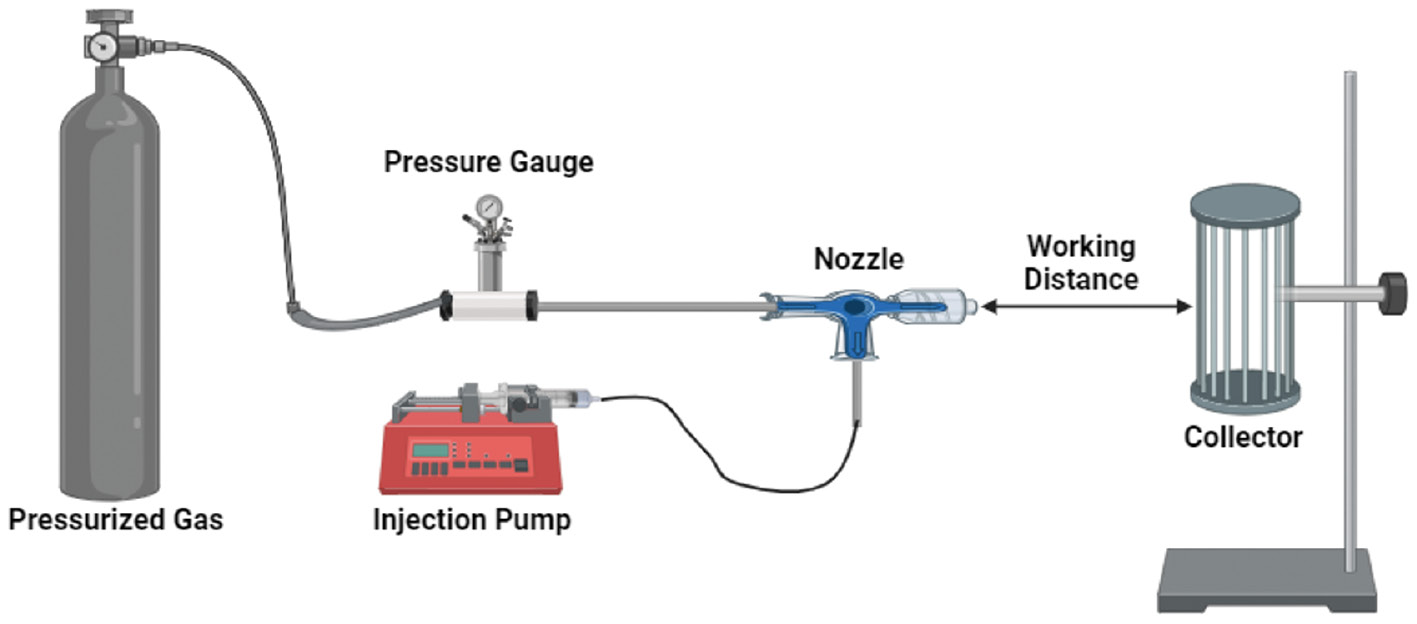
Solution blow spinning
Solution blow spinning (SBS), initially presented by Medeiros et al. in 2009 and also known as air-jet spinning, is a straightforward nanofiber production method that can be easily scaled up. A typical SBS arrangement includes a regulated source of compressed gas, a syringe and pump for delivering the solution to be spun, and a spraying device (Figure 4). In SBS, pressurized gas is used to create nanofibers from a polymer solution. This approach uses a concentric nozzle to deliver the polymer solution and pressurized gas in parallel streams, thus ultimately producing nanofibers [9]. A specialized nozzle with two circular compartments is used in this process. The internal compartment acts as a container for the polymer solution, whereas the external compartment accommodates pressurized gas. The polymer solution is propelled from the nozzle tip by a mix of pressure variance and shear stress at the gas-liquid interface, and the jet is elongated toward the collector. This process results in fiber creation as the solvent evaporates [2]. SBS has emerged as a solution to address several limitations of conventional electrospinning. For instance, SBS enables the in situ synthesis of nanofibers, which is challenging to achieve through electrospinning. Additionally, SBS does not require high electrical potential or conducting targets [6]. Despite the advantages of SBS, the solvents used in its production process can pose certain challenges, such as being toxic, expensive to manufacture, and unsuitable for large-scale production [2].
Figure 4 Solution blow spinning technique for nanofiber formation.
Electrospinning
Electrospinning is a quick and flexible method that uses electrostatic forces to generate extremely delicate polymer fibers that range in size from submicron to nanoscale. By subjecting the polymer liquid (in solution or melt form) to a high-voltage electric field, electrospinning prompts a continuous jet strand to emerge from the dispensing nozzle and accelerate toward the oppositely charged grounded collector [10]. The electrospinning method has several distinctive properties, including affordability, simplicity, high porosity and well distributed pore size, and the ability to yield continuous fibers. This method allows for the use of a wide range of biomaterials to produce nanofibers and requires only minimal amounts of initial solution [11]. Despite its advantages, electrospinning technology requires a strong electric field to produce uniform fibers, thus limiting its efficiency and scalability. Additionally, combining the resulting fibers into an extensive 3D network can be challenging, thus further limiting the popularity and practical applications of this technology [2].
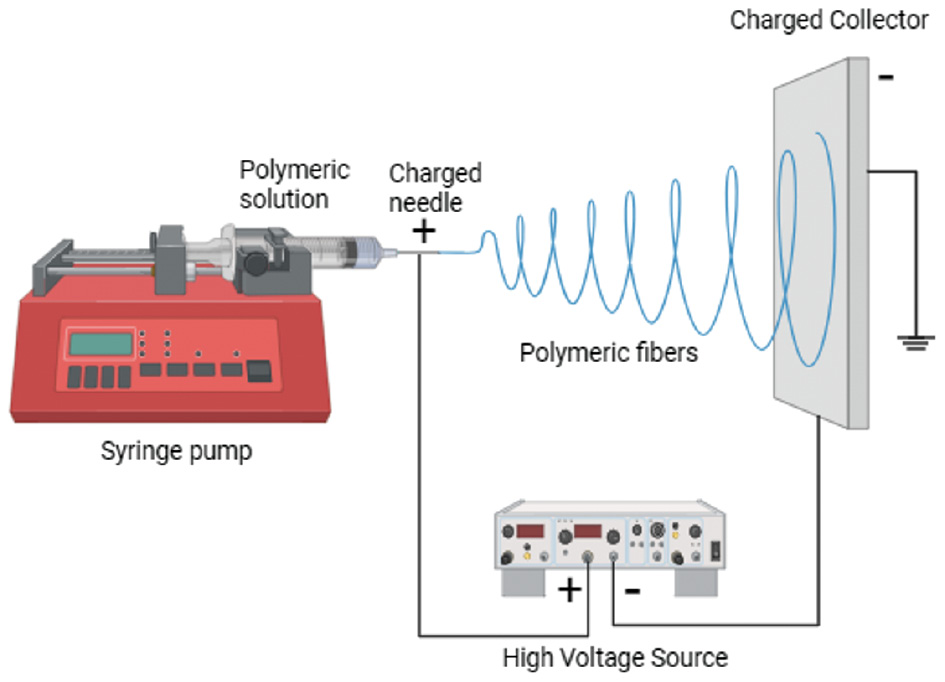
Principle of electrospinning
Electrospinning, originating from “electrostatic yarn,” uses electrostatic forces to create fine fibers, typically ranging from 10 to 100 micrometers and 10 to 100 nanometers in diameter, from a polymer solution or molten polymer [1]. A typical electrospinning setup comprises essential components including a spinneret (or needle), a high-voltage power supply with a broad voltage range, a glass syringe with a fine needle, and a metal collector (Figure 5) [11, 12]. Electrospinning devices use two main configurations: horizontal and vertical setups [13]. During the electrospinning process, high voltage is applied to the syringe to generate an electric field between the syringe needle and the collector, thus facilitating the flow of the spinning fluid [14]. The application of high voltage to the polymer solution induces the polymer solution to accumulate electric charges on its surface. The accumulated charges push against each other until the electric field surpasses the surface tension of the solution. This process leads to the formation of a conical shape known as a Taylor cone. A charged jet is emitted from the top of this cone, and is elongated and stretched under the electric field [12]. As the fiber jets travel through the atmosphere, the solvent contained within them undergoes evaporation, thus resulting in deposition of the solid polymer fibers onto the metal collector [15].
Figure 5 Basic setup of electrospinning device.
The electrospinning process can generally be categorized into four sequential stages:
- A charged liquid droplet results in the development of a conical jet known as a Taylor cone.
- The charged jet undergoes elongation, stretching out in a straight line from the Taylor cone.
- Under the influence of the electric field, the jet’s thickness decreases, thereby playing a role in the creation of more delicate fibers.
- While progressing toward the grounded collector, the electrospinning jet experiences solvent evaporation and solidifies into thin fibers. These fibers are then attracted to the grounded collector and collect on its surface [16].
Materials or nanofiber fabrication
Nanofiber production uses a diverse range of polymers, each selected for its unique characteristics. For drug delivery purposes, a solution of polymer using an appropriate solvent is prepared. An exact amount of drug is added to the polymer solution, thus creating a consistent solution or suspension, depending on the drug’s solubility in the polymer solution. This mixture is then subjected to electrospinning to generate nanofibers composed of a stable polymer-drug complex, and the solvent is eliminated through evaporation during the process [17]. The fundamental building blocks of electrospun nanofibers include natural or synthetic materials, such as polymers, ceramics, and composites [18]. Targeted drug delivery can be achieved by using drug delivery matrices made of either biodegradable or non-degradable polymers. The selection of polymers determines how drugs are released: non-degradable polymers release drugs solely via diffusion, whereas biodegradable polymers involve both matrix erosion and diffusion. Through selection of the appropriate polymers for an electrospun matrix, the rate of drug delivery can be controlled [10]. Table 2 presents polymers and solvents used for the preparation of nanofibers. An ideal biomaterial should exhibit properties such as biocompatibility, ability to undergo natural degradation, absence of toxicity, moderate water-attracting properties, and appropriate mechanical strength [19].
Table 2 Polymers and Solvents Used for Preparation of Therapeutic Nanofibers
| Drug | Polymer/carrier | Solvents | Drug Release Characteristics | Reference |
|---|---|---|---|---|
| Vancomycin | Chitosan, gelatin | Water, glacial acetic acid | Sustained drug release | [30] |
| Tetracycline hydrochloride | PVA, chitosan | Acetic acid solution, water | Initial burst release followed by sustained release | [31] |
| Ciprofloxacin | PLA/GE | Hexafluoro-2-propanol | Initial burst release followed by sustained release | [32] |
| Curcumin | PCL | DCM/ethanol | Slow drug release | [33] |
| Diclofenac sodium | Poly(3-hydroxybutyrate-co-3-hydroxyvalerate) (PHBV) | Hexafluoroisopropanol | Initial burst release followed by controlled release | [34] |
| Progesterone | CMC, PEO | Ethanol | Zero-order drug release | [35] |
| Aspirin | Eudragit (ES100) | Ethanol and N,N-dimethylacetamide | Extended drug release | [36] |
| Rosuvastatin | Chitosan, PCL | Acetic acid | pH-responsive drug release | [37] |
Polymer
Nanofibers acquire distinct attributes as a result of their nanoscale size. Theoretically, a range of polymers can be used to fabricate nanofibers. Table 3 shows various polymers used for the fabrication of nanofibers. Nevertheless, during the development of nanofibers, considering the characteristics of the polymer is essential, because they determine diverse mechanical properties, rate of degradation, and interactions with cellular materials [19].
Table 3 Various Polymers Used for Fabrication of Nanofibers
| Polymer | Properties |
|---|---|
| Natural | |
| Chitosan |
|
| Alginate |
|
| Hyaluronic acid |
|
| Gelatin |
|
| Synthetic polymers | |
| Polyvinyl alcohol |
|
| Polyglycolic acid |
|
| Poly(lactic-co-glycolic acid) and polylactic acid |
|
| Poly(ε-caprolactone) |
|
Solvent
After a suitable polymer with favorable attributes is chosen, the subsequent stage involves creating a polymer dispersion. For successful nanofiber production, the solvent must effectively solubilize the polymer at a concentration suitable for electrospinning. Moreover, the solvents must not undergo any chemical interactions with the dissolved polymer. Water is the preferred solvent, because of its safe and biocompatible nature, but is suitable for only hydrophilic polymers. However, using water as a solvent has several drawbacks. Polymers often exhibit low solubility in water, and the resulting solutions often become thick and viscous at low concentration. Organic solvents, such as acetone, trifluoroethanol, ethyl acetate, acetic acid, ethanol, dichloromethane, tetrahydrofuran, formic acid, dimethylformamide, and methanol are more commonly used in electrospinning [19]. Another important criterion for the selection of solvent is an intermediate boiling point. Volatile solvents are often preferred for electrospinning, because their rapid evaporation rate allows for efficient removal of the solvent from the nanofibers as they travel from the needle tip to the collector. For electrospinning, volatile solvents are usually preferred, but solvents with extremely low boiling points should be avoided. These highly volatile solvents evaporate too rapidly, thereby leading to premature drying of the polymer solution at the needle tip before proper electrospinning into nanofibers can occur. Likewise, solvents with high boiling points should also be avoided. These solvents evaporate too slowly, thus causing the solvent to remain in the nanofibers as they land on the collector and potentially leading to the development of pearl-like structures on the nanofiber surface [20].
Mechanism of drug release
The polymeric network enables drug release via swelling, diffusion, or degradation mechanisms. Factors including the drug properties, polymer composition, interactions, release environment, and preparation method influence drug release from nanofibers [21, 22]. Table 4 outlines the mechanisms of drug release investigated for various polymers.
Table 4 Mechanisms of Drug Release Through Nanofibers
| Polymer | Solvent | Drug | Mechanism of Drug Release | References |
|---|---|---|---|---|
| Polyurethane | Dimethyl formamide | Nigella sativa seed oil | Korsmeyer-Peppas | [38] |
| Polyvinylpyrrolidone | Ethanol | Ciprofloxacin | Korsmeyer-Peppas | [39] |
| Eudragit L100–55, Eudragit S100, and Kollicoat MAE100–55 | Ethanol | Methylprednisolone | Weibull model | [40] |
| Cellulose acetate, poly ɛ-caprolactone | Acetone, dichloromethane, ethanol | Vitamin D3 | Zero-order release | [41] |
| Poly (e-caprolactone), chitosan | Chloroform, methanol, acetic acid, DMSO | Rhodamine B and naproxen | Higuchi model | [42] |
| Polycaprolactone, collagen | Acetic acid | Artemisinin | Korsmeyer-Peppas | [43] |
Scientists have used various mathematical models to assess drug release mechanisms and predict overall release patterns [22]. Various mathematical models have been suggested to explain the kinetics of drug release, including first-order models, the Higuchi model, the Korsmeyer-Peppas model, and the Hixson-Crowell model [23].
Zero-order kinetics
Zero-order release describes the dissolution pattern of a drug from a dosage form in which the drug remains intact and is released gradually. In this mechanism, drug release occurs at a constant rate and is not influenced by the drug concentration within the polymer matrix.
where Qo is the initial amount of drug, Qt is the cumulative amount of drug remaining to be released at time “t,” Ko is the zero-order release constant, and t is time in hours.
The graphical depiction of the proportion of dissolved drugs over time exhibits a linear relationship. The steepness of the line indicates the magnitude of the constant “K” in zero-order release kinetics [22, 24–26].
First-order drug release
A first-order drug release model is used to explain how certain drugs are absorbed or eliminated; the rate at which their concentration changes is directly proportional to the change in time, and depends on the drug concentration within the polymer matrix [22].
where Qo is the initial amount of drug, Qt is the quantity of drug yet to be released at a given time “t,” K is the first-order release constant, and t is the time in hours [26].
When the logarithm of the cumulative percentage of drug remaining is plotted against time, a straight line with a slope of −K/2.303 is obtained.
Higuchi model
Higuchi introduced a mathematical model in 1971 to describe drug dissolution from polymer matrices, primarily for planar systems. This model has since been adapted and modified to accommodate various geometrical systems. The most basic form of the Higuchi model relates drug concentrations to the square root of time [22].
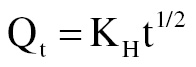
where Qt is the amount of drug remaining to be released at time “t,” and KH is the Higuchi dissolution constant.
Plotting the drug release amount against the square root of time reveals the Higuchi dissolution constant, indicated by the slope of the graph.
This model is applicable only in certain situations, including when (i) the drug concentration exceeds its solubility, (ii) minimal edge effects are present, thus ensuring unidirectional diffusion, (iii) the medium thickness exceeds the drug particle size, (iv) the polymer matrix exhibits minimal swelling or dissolution, (v) the drug diffusion rate remains consistent across the polymer matrix, and (vi) the release environment maintains perfect sink conditions [22].
Hixson-Crowell kinetics model
The Hixson-Crowell model, proposed in 1931, elucidates the relationship between a particle’s surface area and the cube root of its volume [24, 25]. This model is particularly useful for situations in which drug release is affected by changes in particle size and surface area [24].
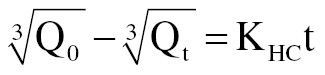
where Q0 is the initial amount of drug, Qt is the amount of drug remained to be released at time “t,” KHC is the Hixson-Crowell release constant, and t is the time in hours.
The Hixson-Crowell model proposes that plotting the cubic root of the initial drug concentration minus the cubic root of the remaining percentage shows a linear relationship over time, thus indicating that the drug release rate is influenced by the surface area of the drug particles [25].
Korsmeyer-peppas model
Korsemeyer and Peppas developed a model in 1983 to study drug release from polymer matrices, including nanofibers. The model presented in this study provides an equation for analyzing release behavior and distinguishing between Fickian and non-Fickian release mechanisms, which are applicable to both swelling and non-swelling polymer matrices. This model uses the initial 60% of the release data to pinpoint and analyze the drug release mechanism [22].
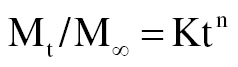
where Mt/M∞ is the portion of the drug that has been released at a given time “t,” K is the rate constant, and n is the diffusion or release exponent.
The diffusional exponent “n” serves to identify and explain the diverse mechanisms governing drug release as interpreted in Table 5 [26].
Table 5 Interpretation of Diffusion Release Mechanisms
| Release Exponent (n) | Drug Transport Mechanism | Drug Release Mechanism |
|---|---|---|
| n < 0.5 | Quasi-Fickian diffusion | Matrix that does not undergo swelling and exhibits diffusion |
| 0.5 | Fickian diffusion | Matrix that does not undergo swelling and exhibits diffusion |
| 0.5 < n < 1.0 | Anomalous (non-Fickian transport) | Diffusion (passive movement) and relaxation/erosion (active breaking down) |
| 1.0 | Case II transport | Concentration-independent drug release |
| > 1.0 | Super case II transport | Matrix erosion-driven drug delivery |
Weibull model
To explain the dissolution and drug release phenomena observed in polymeric networks, Weibull developed an empirical equation in 1951.
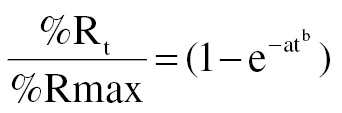
where %Rt is the proportion of drug released at a particular time point, denoted t, %Rmax is the highest percentage released at a specific time point, t, and a and b are the constants characterizing the rate at which drugs are released from their carriers [22].
Peppas-Sahlin model
Peppas and Sahlin developed a new equation in 1989 to measure and describe how drugs are released from polymer matrices. This equation incorporates the swelling capacity of the matrix along with two primary factors that govern the release process [22].
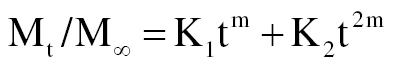
where K1 is the Fickian kinetic constant, and K2 is the erosion rate constant.
Factors affecting the production and morphology of electrospun nanofibers
The electrospinning process is affected by various factors, which can be broadly classified into three main groups: solution characteristics, process conditions, and environmental variables [12–14, 27]. Table 6 summarizes the process parameters for nanofiber preparation.
Table 6 Process Parameters for Nanofiber Preparation
| Category | Requirements | Details |
|---|---|---|
| Solution parameters | Polymer concentration | Optimal concentration to ensure proper viscosity and surface tension for fiber formation (typically 5–20 wt%) |
| Solution viscosity | Affects fiber diameter and morphology; usually in the range of 100–2000 cP | |
| Solution conductivity | Influences the electrospinning process; can be modified by adding salts or ionic compounds | |
| Process parameters | Voltage | Applied voltage between the needle and collector (typically 10–30 kV) |
| Flow rate | Rate at which the polymer solution is fed through the needle (typically 0.5–3 mL/h) | |
| Needle-collector distance | Distance between the needle and the collector (typically 10–20 cm) | |
| Collector type | Type of collector used (e.g., stationary, rotating drum, or rotating disc) affecting fiber alignment and morphology | |
| Environmental conditions | Humidity | Relative humidity affecting fiber morphology and pore structure (usually 30–50%) |
| Temperature | Ambient temperature influencing solution properties and fiber formation (usually 20–30°C) |
Solution parameters
Effect of molecular weight
The polymer’s molecular weight directly correlates with solution viscosity, rheology, flexibility, and degree of chain entanglement, and is inversely proportional to chain entanglement [12]. As the polymer solution moves from the needle tip to the collector during the electrospinning process, it undergoes a stretching phenomenon. The entangled network of polymer chains prevents the fragmentation of the electrically charged jet, thus enabling uninterrupted flow of the solution [28]. A greater degree of entanglement results in increased drag and intermolecular attraction [21]. Higher molecular weight decreases the tendency of polymer solutions to form beads and causes an enlargement of pore size, thus resulting in the formation of a consistently meshed structure [27].
Effect of solution viscosity
A clear correlation exists between the viscosity of the polymer solution and the polymer concentration [12]. To create polymer fibers with larger diameters, viscosity can be increased by raising either the polymer concentration or its molecular weight [27]. Increased solution viscosity also leads to increased entanglement among polymer chains. Because of entanglement, the beads transform from spherical to spindle-shaped structures and ultimately develop into smooth fibers [13]. In contrast, when a polymer solution exhibits excessively high viscosity, jet formation becomes difficult, because the flow of polymer at the needle tip is obstructed [27]. The ideal viscosity range for spinning is typically between 1 and 200 poise. However, uniform nanofibers can be produced specifically at viscosities ranging from 1 to 20 [13].
Effects of polymer concentration
For chain entanglement to occur in the polymer solution, the polymer concentration must be maintained within a specific range that is neither too dilute nor too concentrated. Achieving continuous fiber production substantially relies on the appropriate selection of polymer concentration, taking into account factors such as viscosity and surface tension [27]. Thus, the polymer solution should not be too diluted, the viscosity is decreased, and the surface tension is increased. Subsequently, a loss of intermolecular attractions within the charged jets causes them to break into individual droplets as they emerge from the Taylor cone [13]. Similarly, excessive concentrations, which would prevent the formation of fibers altogether, must be avoided [3].
Effects of surface tension
Surface tension decreases the surface area per unit mass of a fluid [28]. Overcoming this surface tension is essential to start the electrospinning process by using the given solution [13]. Free solvent molecules present in high concentrations tend to aggregate and form spheres because of surface tension [28]. Decreased surface tension promotes greater interaction among the solvent molecules and polymers. This enhanced interaction allows the solvent molecules to evenly disperse across the entwined polymer molecules and leads to the formation of smooth fibers without beads [13]. Surface-active agents can be used to manipulate surface tension. However, lowering surface tension alone is not sufficient to address the issues that arise from using a polymer with low molecular weight [19].
Effects of solution conductivity
Electrospinning is a process involving the stretching of a solution, because of the repulsion between charges on its surface. Consequently, increasing the solution’s conductivity enables the electrospinning jet to carry a greater number of charges [28]. The conductivity of the electrospinning solution is influenced by several factors, such as the type of polymer, the solvent used, and the presence of ionic salts. Higher solution conductivity leads to the formation of thinner fibers, whereas lower conductivity results in thicker fibers. Polymer solutions with high conductivity exhibit instability under strong electric fields, thus leading to the occurrence of bending instability [12]. The addition of salt results in the production of finer and more uniform fibers, and simultaneously decreases bead formation. The increased elongation and dielectric stresses experienced by the polymer jet experiences are attributable to a rise in charge density. Consequently, thinner fibers are formed [27].
Effects of solvent volatility
For effective electrospinning, the solvent should completely dissolve the polymer and form a uniform solution. The solvent should also exhibit moderate volatility, characterized by a moderate boiling point. Solvents with high volatility and low boiling points are not recommended for electrospinning, because of their tendency to evaporate quickly at the needle tip, thus leading to blockages and hindering the electrospinning process. Similarly, avoiding non-volatile solvents is also important, because they prevent the nanofibers from drying fully when they reach the collector, thus causing bead formation [12]. Before solid fibers form on the collector plate, phase separation occurs as the fiber jet is released from the capillary tube. The extent of this separation is largely influenced by the solvent’s volatility [3].
Effect of the dielectric constant of the solvent
Electrospinning with solutions having higher dielectric constants results in greater bending instability, which in turn contributes to the formation of thinner nanofibers and suppresses bead formation. Additionally, an increased area of deposition results [21]. Solvents with higher dielectric constants typically exhibit higher net charge density. Therefore, in the electrospinning process, these solvents apply increased elongation forces to the charged jet, thereby leading to decreased bead formation and thinner fiber diameters. To enhance the dielectric properties of the electrospinning solution, various solvents such as toluene, ethanol, acetone, m-cresol, acetic acid, dimethylformamide, chloroform, tetrahydrofuran, acetonitrile, dichloromethane, and ethyl acetate can be used [13].
Processing parameters
Effects of voltage
A voltage of appropriate magnitude is necessary to initiate jet formation, primarily according to the characteristics of the solution, such surface tension and viscosity. An adequate voltage level is required to initiate jet formation, and is largely influenced by solution characteristics including viscosity and surface tension. Insufficient voltage fails to generate the necessary electrostatic forces to overcome droplet surface tension. Consequently, the jet fails to stretch out, thus leading to the formation of droplets instead. Elevating the voltage beyond a specific threshold initiates the formation of the jet, and causes heightened whipping and instability in the fibers. Consequently, the fiber jet undergoes elongation [14]. Researchers are in disagreement regarding the influence of applied voltage on the diameter of electrospun fibers. Although some studies have suggested that the fiber diameter increases as the applied voltage rises, others have concluded that the effect of applied voltage on electrospun fiber diameter is negligible. Interestingly, several research groups have even documented the decrease in fiber diameter as the applied voltage is raised. These seemingly contradictory findings can be clarified by considering the following. When the voltage increases in electrospinning, two effects on fiber diameter are observed. First, higher voltage ejects more polymer solution, thereby forming an initial jet with a larger diameter and consequently promoting the generation of fibers with greater diameter. In contrast, applying a higher voltage amplifies the density of surface charges on the initial jet, thus causing the jet to divide into smaller jets, and yielding fibers with smaller diameters. Both these effects can occur simultaneously. When the first effect is dominant, thicker fibers are produced. In contrast, when the second effect takes precedence, thinner fibers are produced [28].
Effects of flow rate
Fiber size, porousness, and organization are affected by the rate at which the polymer solution flows. Higher flow rates result in larger fiber diameters. In contrast, using a slower flow rate allows for the creation of thinner fibers, which are desirable because they provide adequate time for solvent evaporation. However, beading occurs in the fibers at higher flow rates, because of rapid solvent evaporation [27].
Separation between the needle tip and the collector
To achieve the desired morphology and dimensions of electrospun nanofibers, adjusting the distance between the needle tip and the collector is essential [17]. The optimal distance between the collector plate and the needle tip is essential, because a decrease in this distance results in a shorter flight time. That is, insufficient time for solvent evaporation may occur and potentially lead to bead defects [3].
Needle diameter
The diameter and structure of the resulting nanofibers are substantially influenced by the internal diameter of the needle used during electrospinning [12]. When the orifice diameter decreases, the resulting fibers also have a smaller diameter, because of the limited solution accumulation at the end of the capillary tube caused by the decreased orifice size [3].
Effects of the collector
The choice of collector material substantially influences the electrospinning process, because it serves as the conductive surface that attracts and collects the charged nanofibers. Although aluminum foil is frequently used as a collector, detaching electrospun nanofibers from it can be challenging. Additionally, alternative electrodes, such as conductive cloth, gridded bar, mesh, pin, parallel or paper, rotating wheel, and rotating rod electrodes, are occasionally devised to facilitate the production of aligned fibers [12]. When a non-conductive collector is used, the similar charges on the fibers repel each other, thus decreasing deposition and occasionally leading to the formation of three-dimensional fibers. A porous collector accelerates solvent evaporation, whereas a patterned collector alters the texture of the fiber mat. In contrast, a rotating collector provides an enhanced morphology by allowing more time for solvent evaporation [21].
Environmental parameters
Despite advancements in electrospinning technology, the influence of ambient conditions on the process has not been thoroughly investigated. These conditions include the following:
Humidity
Humidity influences the structure of fibers and leads to pore formation on the surfaces of the fibers as humidity rises. By manipulating the humidity levels, modified electrospun nanofibers can be created [12]. This phenomenon occurs because water droplets generated during electrospinning condense on the polymer’s surface and subsequently form pores as they dry [21]. In conditions with very low humidity, the rapid evaporation of solvents can disrupt the electrospinning process and potentially cause needle tip blockage [12].
Temperature
The speed of solvent evaporation and the viscosity of a polymer solution or melt are affected by the ambient temperature. Higher ambient temperatures lead to faster solvent evaporation and cause the formation of thicker nanofibers. In contrast, lower environmental temperature decreases the solvent evaporation rate and leads to formation of thinner nanofibers [19]. When the ambient temperature is elevated, the polymer jet’s splaying and elongation process cannot be fully accomplished, because of faster solidification rates [28]. Moreover, as the polymer solution’s viscosity decreases, a greater degree of fiber stretching occurs. This increased stretching results in thinner fibers [13]. Using elevated temperatures leads to loss of functionality in biopolymers such as proteins and enzymes [21].
Applications of nanofibers in drug delivery
Nanofibers have shown substantial promise in the field of drug delivery, because of their unique properties, such as high surface area, porosity, and tunable release profiles. Table 7 lists the therapeutic applications of nanofibers.
Table 7 Therapeutic Applications of Nanofibers
| Application | Materials for Nanofibers | Therapeutic Agent | Description | Reference |
|---|---|---|---|---|
| Antiviral drug delivery | Acyclovir/hydroxypropyl-beta-cyclodextrin (HP-βCD) | Acyclovir | To overcome acyclovir’s low water solubility and low bioavailability, a polymer-free and fast dissolving drug delivery system was designed by complexing acyclovir with HP-βCD. The drug/cyclodextrin complex was then formulated as nanofibers for oral delivery. | [44] |
| Multi antimicrobial activity | Chitin | Silver nanoparticles | Sheets of chitin nanofibers embedded with silver nanoparticles exhibited antimicrobial effects against H1N1 influenza A virus, Escherichia coli, and Pseudomonas aeruginosa. | [45] |
| Floating gastro-retentive drug delivery system | Tripolyphosphate-crosslinked chitosan/poly (ethylene oxide) | Ranitidine hydrochloride | Drug embedded nanofibrous mats formulated with tripolyphosphate-crosslinked chitosan/poly (ethylene oxide) increased the bioavailability and mucoadhesive properties because of gastric retention. | [46] |
| Anticancer drug delivery | Poly (ε-caprolactone diol), polyurethane | Temozolomide | Poly (ε-caprolactone diol)-based polyurethane (PCL-diol-b-PU) nanofibers were created by integrating chitosan nanoparticles loaded with a drug. The nanofibers facilitated sustained delivery of the drug, thereby treating glioblastoma cancer. | [47] |
| Face mask | Polypropylene | Polyvinylidene fluoride (PVDF)/titanium nanotube (TNT) nanofibers | A face mask designed for air purification from bacterial contamination was created by weaving electrospun nanofibers made of polyvinylidene fluoride and incorporating titanium nanotubes. | [48] |
| Wound dressing | Polycaprolactone/chitosan | Aloe vera | The nanofiber membrane formulation exhibited outstanding antibacterial properties and compatibility with biological systems, thus facilitating wound healing. | [49] |
| Wound dressing | Poly(D,L-lactide) (PDLLA) and poly(ethylene oxide) (PEO) | Nisin, 2,3-dihydroxybenzoic acid (DHBA) | Adding DHBA and nisin to the nanofiber increased the dressing’s antimicrobial activity. The improvement was associated primarily with DHBA’s ability to chelate iron and destabilize the cell membrane of the target organism. | [50] |
| Orthopedic implant-associated infections | Poly(D,L-lactic acid-co-glycolic acid) (PLGA) | Fusidic acid, rifampicin | Electrospun biodegradable PLGA nanofibers loaded with a combination of drugs showed a biphasic release pattern and localized delivery of antibiotics to prevent infection. | [51] |
| Hemorrhage control (antifibrinolytic) application | Polyvinyl alcohol/chitosan | Tranexamic acid | Patches with a combination of an antifibrinolytic agent and antibacterial hemostatic polymer had excellent potential in the management of hemostasis. | [52] |
| NSAID drug delivery | Zein/Eudragit | Aceclofenac/pantoprazole | Nanofibers were created to overcome the drawbacks of non-steroidal anti-inflammatory drugs (NSAIDs). | [53] |
| Anticancer drug delivery | Polycaprolactone/chitosan | 5-fluorouracil | Nanofibers containing 5FU, formed through the combination of polycaprolactone (PCL) and chitosan (CS), exhibited effective therapeutic properties and diminished systemic adverse effects by targeting specific sites by taking advantage of the acidity around cancer cells and the pH sensitivity of chitosan. | [54] |
| Acute pain relief | Poly(vinyl alcohol) (PVA) and poly(vinyl pyrrolidone) (PVP) | Buprenorphine hydrochloride | Transdermal patches of buprenorphine provided sustained drug release, and improved bioavailability and ease of administration. | [55] |
| Treatment of periodontitis | Poly (D-L) lactide-co-glycolide (PLGA) and poly ε-caprolactone (PCL) | Metronidazole and amoxicillin | Metronidazole- and amoxicillin-loaded PLGA and PCL nanofibers provided a prolonged release profile, thus improving patient compliance by decreasing the dosing frequency. | [56] |
| Cervical cancer treatment | Polyvinyl alcohol/polycaprolactone (PVA/PCL) | Doxorubicin | Nanofibers with a core-shell structure comprising PVA/PCL, exhibited prolonged and pH-sensitive drug release, thus offering potential for treating cervical cancer and other solid malignancies. | [57] |
| Treatment of osteoarthritis | Poly (ethylene glycol) diacrylate (PEGDA)-1, 2-ethanedithiol (EDT) copolymer | Fucoxanthin | A nanofiber membrane made from PLA/PEGDA-EDT@rGO-fucoxanthin was developed by integrating PEGDA-EDT as a responsive element to reactive oxygen species (ROS); reduced graphene oxide served as a carrier for drugs, and fucoxanthin served as an agent with antioxidative and anti-inflammatory properties. These components were introduced into the PLA matrix to enable targeted and sustained drug release, specifically designed for osteoarthritis therapy. | [58] |
| Treatment of inflammatory bowel disease | Polymethacrylate and different grades of Eudragit | Budesonide | Nanofibers designed for colon targeting exhibited sensitivity to pH changes and time-dependent characteristics. | [59] |
| Regenerative endodontics | Poly(vinylpyrrolidone) (PVP) | Ciprofloxacin (CIP), minocycline (MINO), and metronidazole (MET) | Nanofibers containing a combination of antibiotics were formulated for disinfecting bacteria in decaying teeth before initiation of regeneration. | [60] |
| Chronic fungal infections | Polycaprolactone, gelatin | Terbinafine hydrochloride | Formulated fibers were effective against Trichophyton mentagrophytes and Aspergillus fumigatus, exhibited strong antifungal activity, and can be used to treat chronic recurrent dermatophytosis. | [61] |
| Delivery of antiviral agents | Poly(lactic-co-glycolic acid) (PLGA) | Griffithsin | Griffithsin-modified electrospun fibers effectively inhibited in vitro HIV infection. | [62] |
| Diabetic foot ulcer infection | Gelatin/polyvinyl alcohol | Vancomycin, imipenem/cilastatin | A dual drug-loaded core-shell nanofibrous mat had excellent antibacterial activity. | [63] |
Patent and current clinical trial status of nanofibers
Nanofibers have emerged as a promising technology in the field of drug delivery systems, and their unique properties—such as high surface area-to-volume ratio, tunable porosity, and the ability to encapsulate a wide range of therapeutic agents—have been leveraged. These characteristics make nanofibers highly effective in enhancing drug solubility, stability, and controlled release profiles. The patent landscape for nanofiber-based drug delivery systems is rapidly evolving, reflecting growing interest and innovation in this area. Table 8 lists patents on nanofibers. Concurrently, clinical trials are underway to evaluate the safety, efficacy, and potential applications of these advanced drug delivery platforms in various therapeutic domains. Nanofiber formulations in clinical trials are listed in Table 9. Understanding the current patent status and clinical trial progress is crucial for stakeholders in the pharmaceutical and medical research fields, to provide insights into the technological advancements and regulatory milestones influencing the development and commercialization of nanofiber-based drug delivery systems.
Table 8 Patents Filed on Nanofibers
| Patent Number | Title | Findings of Invention/summary | References |
|---|---|---|---|
| IN202221071107 | Nanodispersion loaded nanofibers formulation for the treatment of vulvo-vaginal candidiasis | Posaconazole, an antifungal for severe Candida and Aspergillus infections, is formulated into nanofibers for extended vaginal drug release. These uniform, non-beaded, non-woven nanofibers ensure sustained release of posaconazole. | [64] |
| IN202341004551 | Preparation and evaluation of drug loaded nanofiber | The invention describes polymeric nanofibers made from starch or polyethylene oxide, loaded with ibuprofen or ketoprofen. These nanofibers enhance the solubility and bioavailability of poorly water-soluble NSAIDs. They are produced via centrifugal spinning, and have been tested for drug release, morphology, chemical structure, and tensile strength. | [65] |
| IN202321003119 | Glycyrrhizin loaded nanofiber topical drug delivery for management of chronic wounds | The invention creates glycyrrhizin-loaded nanofibers for treating chronic wounds. These fibers, made from glycyrrhizin and PVA, offer high drug entrapment (99.27%) and loading efficiency (82.4%). They provide sustained drug release; enhance wound healing; and have antibacterial, antioxidant, and biocompatible properties, thus making them ideal for chronic wound management. | [66] |
| IN202221030754 | Construction of curcumin-bael fruit gum electrospun nanofibers | The invention creates nanofibers using curcumin and bael fruit gum (BFG) with electrospinning, incorporating polyvinyl alcohol (PVA) for stability. These nanofibers are highly effective for drug delivery, particularly in wound dressings, owing to their fine morphology and high therapeutic efficiency. Curcumin provides antioxidant and antibacterial properties, whereas BFG enhances solubility and adds anti-inflammatory benefits. | [67] |
| WO2020208619 | Colchicine loaded nanofibers: preparation method, characterization, optimization, and related applications | The invention introduces a nanofiber-based drug delivery system for colchicine, enabling safer and more effective topical and transdermal administration. It addresses various dermatological and systemic conditions while also showing promise in cancer therapy as a neoadjuvant and adjuvant treatment to prevent tumor recurrence. | [68] |
| US20200289416 | Drug delivery vehicles for atherosclerosis nanomedicine | The invention introduces peptide amphiphiles and nanofibers for treating atherosclerosis. Peptide amphiphiles include a hydrophobic tail, structural and charged peptide segments, and a targeting peptide or therapeutic agent. Nanofibers made from these peptide amphiphiles can target atherosclerotic lesions and deliver therapeutic agents effectively, thus offering promising treatment options. | [69] |
| EP3016613 | Bio-compatible apitherapeutic nanofibers | The invention introduces a nanofibrous scaffold made from polymers such as chitosan, offering a high porosity and surface-to-volume ratio. It can include various additives such as antimicrobial agents, natural extracts, antibiotics, and anticancer drugs, enabling diverse applications including drug delivery and wound dressing. | [70] |
| US20160130390 | Hyperbranched amino acid-based poly(ester urea)s for regenerative medicine and drug delivery | The invention introduces hyperbranched amino acid-based poly(ester urea) (PEU) polymers for regenerative medicine and drug delivery. These polymers have adjustable properties and can withstand ethylene oxide sterilization without degrading. They consist of linear and branched segments with various amino acid residues, and form durable nanofibers or microfibers through electrospinning and other methods. | [71] |
| CN112843088 | Double-drug-loading electrostatic spinning nanofiber scaffold and preparation method and application thereof | The invention is a double-drug-loading electrostatic spinning nanofiber scaffold made from PCL nanofibers loaded with curcumin (CUR) and coated with a polydopamine (PDA) membrane embedded with selenium nanoparticles (SeNPs). This scaffold has good biocompatibility and pH responsiveness, and can effectively release both anti-cancer drugs, thereby promoting skin tissue healing and resisting tumors while decreasing chemotherapy toxicity and drug resistance. | [72] |
| US20150037390 | Self-assembling bis-urea compounds for drug delivery | The invention features cationic fibers for encapsulating and delivering hydrophobic anionic drugs, offering reversible binding and controlled release. These fibers enhance drug stability, solubility and decrease toxicity, thus making them suitable for targeted drug delivery, such as in cancer treatment. | [73] |
| EP2632493 | Drug delivery compositions | The invention introduces a novel drug delivery method using cellulose nanofibers or derivatives in a hydrogel matrix. These hydrogels, derived from plant cellulose, offer even drug distribution without additives and are injectable, and therefore hold promise for medical applications. | [74] |
| WO2005025630 | Polymeric nanofibers for tissue engineering and drug delivery | Polymeric nanofibers, made from various degradable and non-degradable polymers, are developed for medical and other uses, including drug delivery, tissue engineering, and protective clothing. Notably, these polymers include polyphosphazenes and their composites with nanosized particles like hydroxyapatites. | [75] |
| US20140128345 | Vaginal matrices: nanofibers for contraception and prevention of HIV infection | The invention involves electrospun fiber compositions that contain at least two different drugs with diverse physicochemical properties. These fibers can be used for applications including implants or mucosal contact, particularly for simultaneously delivering antimicrobial and contraceptive agents to the vaginal mucosa, thereby protecting against infections and preventing unintended pregnancies. | [76] |
| CN114000262 | Drug-loaded polydopamine coated nanofiber dressing and preparation method thereof | The invention is a wound dressing made from polycaprolactone nanofibers coated with polydopamine and loaded with epsilon-polylysine. It offers antibacterial, photothermal, and antioxidant properties. The preparation is simple and non-toxic, and experiments confirmed its effectiveness and safety for wound care. | [77] |
Table 9 Nanofibers in Clinical Trials
| Sr.no. | Study Title | Interventions/Treatments | Use (Disease and Formulation) | Clinical Trial Identifier |
|---|---|---|---|---|
| 1 | Antimicrobial effect of modified antibiotic nanofibers for regenerative endodontics procedures | Procedure: electrospun triple antibiotic mixture nanofibers Procedure: modified triple antibiotic mixture paste |
Pulp necrosis | NCT03690960, 01 October 2018 [78] |
| 2 | Investigating the efficacy of insert nanofibers containing vancomycin and amikacin in patients with infectious keratitis | Interventions 1: 0.5% tetracaine drops + nanofiber containing vancomycin-amikacin + artipic advanced artificial tears 0.15% Intervention 2: fort vancomycin (50 mg/ml) and one drop of fort amikacin (20 mg/ml) |
Corneal ulcer | IRCT20130812014333N216, 10 May 2024 [79] |
| 3 | Synthesis and evaluation of the effect of F. vulgaris nanofibers on burn wounds | Intervention 1: nanofibers containing Pagaze plant extract (at least 1 mg/cm2) Intervention 2: nanofibers without Pagaze extract Intervention 3: control group |
Second degree burn injury | IRCT20130722014106N10, 05 August 2023 [80] |
| 4 | Effect of colchicine on aphthous ulceration | Intervention 1: nanofiber mat Intervention 2: control group |
Aphthous recurrent oral aphthae | IRCT20160920029889N4, 07 January 2023 [81] |
| 5 | Clinical study of a new liposome nanofiber patch for transdermal drug delivery containing ebracteolata Hayata in the treatment of actinic keratosis | Intervention 1: drug loaded nanofibrous patch Intervention 2: placebo |
Actinic keratosis | ChiCTR2000036997, 26 August 2020 [82] |
| 6 | Clinical study of functional electrospun nanofibers capturing circulating patient tumor cells to predict the efficacy and prognosis of patients with ovarian cancer | Gold standard: clinical outcome; index test: CTCs of patients with ovarian cancer at different stages, captured by electrospinning nanofibers | Ovarian cancer | ChiCTR2000037343, 28 August 2020 [83] |
| 7 | SVF combined with functional self-assembling peptide nanofiber hydrogels in the treatment of spinal cord injury | Procedure: stromal vascular fraction (SVF) combined with functional self-assembling peptide nanofiber hydrogels | Traumatic spinal cord injury | NCT05967325, 01 August 2023 [84] |
| 8 | Novel silk fibroin nanofiber membrane using minimally invasive surgery in treatment of periodontal intrabony defects: a randomized clinical trial | Procedure: minimally invasive surgery technique (MIST) + novel silk fibroin (SF) nanofiber membrane Procedure: MIST + collagen membrane Procedure: MIST |
Intrabony periodontal defect | NCT06371027, 17 April 2024 [85] |
| 9 | Effect of a mixture of doxycycline and venlafaxine on the healing of diabetic foot ulcers | Intervention 1: nanofibers containing doxycycline and venlafaxine Intervention 2: control group |
Treatment of diabetic foot ulcer; type 2 diabetes mellitus with circulatory complications | IRCT20160711028878N2, 01 February 2020 [79] |
Challenges and future prospects
The development of diverse nanofiber production methods has resulted in substantial advancements in creating multiple platforms for drug delivery technologies [14]. Creating nanofibers is markedly more expensive than creating traditional fibers, because of expensive technologies involved and lower production rates [3]. Leading research on centrifugal spinning, pressure gyration, electrospinning, and solution-blowing is progressing toward large-volume production. Certain systems such as NanoSpinner416n and FibeRio® Technology are already being used industrially. These high-tech systems have shown great promise in the production of homogeneous and continuous fibers. However, a challenge lies in ensuring that fibers are produced with the required morphological, mechanical, and chemical characteristics, particularly during large-volume production [14]. Another major obstacle involves achieving efficient production of nanofibers that adhere to universally recognized standards and comply with stringent regulatory requirements. To address this concern effectively, various aspects, including environmental safety, reproducibility, accuracy, and the ability to meet market demands through large-scale production, must be successfully managed [29]. Comprehensive pre-clinical and clinical assessments are crucial for the successful transition of these products from the laboratory to the market [14]. These assessments will require the establishment of regulations and global standards to evaluate the environmental impact of both the products and their by-products, as well as their in vivo toxicity and biocompatibility [29].
Conclusion
Electrospinning is a straightforward technique used in both laboratory and industrial settings to produce nano-scale fibers. Nanofibers, owing to their size, have special physical properties that render them appropriate for diverse domains and applications. Among the numerous available production techniques, electrospinning is an extensively researched and widely used technique. This process allows for constructing nanofibers from various materials, such as polymers, carbon, metal oxides, and composites. These nanofibers have unique traits such as a large surface area, surface functionality, interconnected pores, and flexibility. Their shape is affected by solution properties, manufacturing methods, and environmental factors; optimizing these variables yields uniform nanofibers. Despite their immense potential, nanofibers still encounter limitations in tissue engineering applications. Electrospun nanofibrous scaffolds face challenges, including that small pore sizes hinder cell growth, and their mechanical properties are often unsuitable for hard tissue regeneration. Addressing these issues during application and managing in vivo degradation pose additional challenges. Nevertheless, nanofibers are becoming commonly used for delivering drugs because of their special qualities, including precise targeting, the ability to hold many drugs, high efficiency in encapsulating drugs, enhanced drug effectiveness, and diminished adverse effects. They hold great promise in various biomedical applications, particularly for treating bacterial biofilms and infections associated with orthopedic implants, and providing tissue scaffolds and wound dressings. To further enhance the potential of nanofibers, efforts should focus on developing diverse properties and high-throughput manufacturing techniques. By addressing these aspects, nanofibers may revolutionize multiple industries and contribute to groundbreaking advancements in various fields.
Literature search strategy
A comprehensive literature search was conducted to identify relevant studies. The following databases were searched: PubMed, Scopus, and Google Scholar. The primary databases used for patent searches were Google Patents, Espacenet, World Intellectual Property Organization, and the United States Patent and Trademark Office (USPTO) database. Clinical trial information was sourced from ClinicalTrials.gov. The search was performed with the following keywords: “Nanofibers,” “Nanofibers for drug delivery,” “Fabrication of Nanofibers,” and “applications.” The search was limited to articles published in English between May 2010 and April 2024.
Conflict of interest
The authors declare that there are no conflicts of interest.
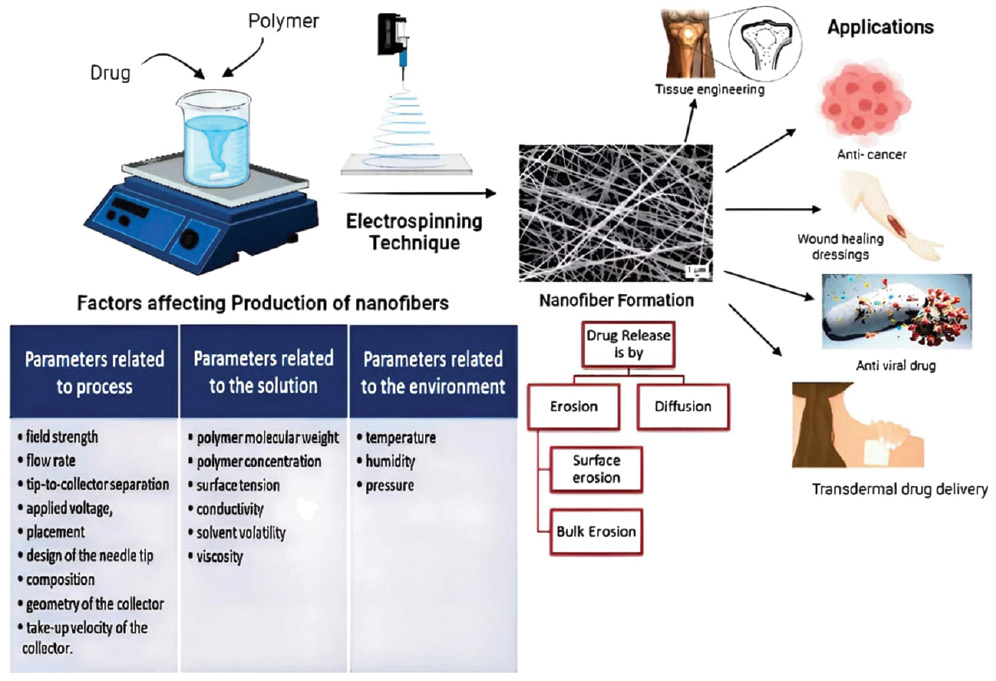
Graphical abstract
The graphical abstract illustrates the creation of drug-loaded nanofibers emphasizing the impact of process, solution, and environmental parameters on nanofiber formation. These nanofibers, known for their extensive surface area, are applied in tissue engineering, cancer therapy, wound healing, antiviral treatments, and transdermal drug delivery. The release of drugs from the nanofibers occurs through mechanisms like erosion and diffusion, highlighting their potential in advanced medical applications.
References
- Torres-Martínez EJ, Pérez-González GL, Serrano-Medina A, Grande D, Vera-Graziano R, et al. Drugs loaded into electrospun polymeric nanofibers for delivery. J Pharm Pharm Sci 2019;22:313-31. [PMID: 31329535 DOI: 10.18433/jpps29674]
- Duan X, Chen HL, Guo C. Polymeric nanofibers for drug delivery applications: a recent review. J Mater Sci Mater Med 2022;33(12):78. [PMID: 36462118 DOI: 10.1007/s10856-022-06700-4]
- Morie A, Garg T, Goyal AK, Rath G. Nanofibers as novel drug carrier–an overview. Artif Cells Nanomed Biotechnol 2016;44(1):135-43. [PMID: 25016918 DOI: 10.3109/21691401.2014.927879]
- Lou L, Osemwegie O, Ramkumar SS. Functional nanofibers and their applications. Ind Eng Chem Res 2020;59(13):5439-55. [DOI: 10.1021/acs.iecr.9b07066]
- Alghoraibi I, Alomari S. Different methods for nanofiber design and fabrication. Handbook of Nanofibers. 2018;1:46. [DOI: 10.1007/978-3-319-42789-8_11-2]
- Kenry X, Lim CT. Nanofiber technology: current status and emerging developments. Prog Polym Sci 2017;70:1-7. [DOI: 10.1016/j.progpolymsci.2017.03.002]
- Raimi-Abraham BT, Mahalingam S, Davies PJ, Edirisinghe M, Craig DQ. Development and characterization of amorphous nanofiber drug dispersions prepared using pressurized gyration. Mol Pharmaceutics 2015;12(11):3851-61. [DOI: 10.1021/acs.molpharmaceut.5b00127]
- Mahalingam S, Edirisinghe M. Forming of polymer nanofibers by a pressurised gyration process. Macromol Rapid Commun 2013;34(14):1134-9. [PMID: 23749758 DOI: 10.1002/marc.201300339]
- Dadol GC, Kilic A, Tijing LD, Lim KJ, Cabatingan LK, et al. Solution blow spinning (SBS) and SBS-spun nanofibers: materials, methods, and applications. Mater Today Commun 2020;25:101656. [DOI: 10.1016/j.mtcomm.2020.101656]
- Pillay V, Dott C, Choonara YE, Tyagi C, Tomar L, et al. A review of the effect of processing variables on the fabrication of electrospun nanofibers for drug delivery applications. J Nanomater 2013;2013: 1-22. [DOI: 10.1155/2013/789289]
- Eatemadi A, Daraee H, Zarghami N, Melat Yar H, Akbarzadeh A. Nanofiber: synthesis and biomedical applications. Artif Cells Nanomed Biotechnol 2016;44(1):111-21. [PMID: 24905339 DOI: 10.3109/21691401.2014.922568]
- Ibrahim HM, Klingner A. A review on electrospun polymeric nanofibers: production parameters and potential applications. Polym Test 2020;90:106647. [DOI: 10.1016/j.polymertesting.2020.106647]
- Islam MS, Ang BC, Andriyana A, Afifi AM. A review on fabrication of nanofibers via electrospinning and their applications. SN Appl Sci 2019;1:1-16. [DOI: 10.1007/s42452-019-1288-4]
- Farhaj S, Conway BR, Ghori MU. Nanofibres in drug delivery applications. Fibers. 2023;11(2):21. [DOI: 10.3390/fib11020021]
- Zhao Y, Qiu Y, Wang H, Chen Y, Jin S, et al. Preparation of nanofibers with renewable polymers and their application in wound dressing. Int J Polym Sci 2016;2016:1-17. [DOI: 10.1155/2016/4672839]
- Xue J, Wu T, Dai Y, Xia Y. Electrospinning and electrospun nanofibers: methods, materials, and applications. Chem Rev. 2019;119(8):5298-415. [DOI: 10.1021/acs.chemrev.8b00593]
- Torres-Martínez EJ, Cornejo Bravo JM, Serrano Medina A, Pérez González GL, Villarreal Gómez LJ. A summary of electrospun nanofibers as drug delivery system: drugs loaded and biopolymers used as matrices. Curr Drug Deliv 2018;15(10):1360-74. [PMID: 30033869 DOI: 10.2174/1567201815666180723114326]
- Manea LR, Hristian L, Leon AL, Popa A. Recent advances of basic materials to obtain electrospun polymeric nanofibers for medical applications. IOP Conf. Ser.: Mater. Sci. Eng. 2016;145(3):032006. IOP Publishing. [DOI: 10.1088/1757-899X/145/3/032006]
- Pelipenko J, Kocbek P, Kristl J. Critical attributes of nanofibers: preparation, drug loading, and tissue regeneration. Int J Pharm 2015;484(1-2):57-74. [PMID: 25701683 DOI: 10.1016/j.ijpharm.2015.02.043]
- Haider A, Haider S, Kang IK. A comprehensive review summarizing the effect of electrospinning parameters and potential applications of nanofibers in biomedical and biotechnology. Arab J Chem 2018;11(8):1165-88. [DOI: 10.1016/j.arabjc.2015.11.015]
- Gaydhane MK, Sharma CS, Majumdar S. Electrospun nanofibres in drug delivery: advances in controlled release strategies. RSC Adv 2023;13(11):7312-28. [DOI: 10.1039/D2RA06023J]
- Abdul Hameed MM, Mohamed Khan SA, Thamer BM, Rajkumar N, El-Hamshary H, et al. Electrospun nanofibers for drug delivery applications: methods and mechanism. Polym Adv Technol 2023;34(1):6-23. [DOI: 10.1002/pat.5884]
- Cleeton C, Keirouz A, Chen X, Radacsi N. Electrospun nanofibers for drug delivery and biosensing. ACS Biomater Sci Eng 2019;5(9):4183-205. [DOI: 10.1021/acsbiomaterials.9b00853]
- Dash S, Murthy PN, Nath L, Chowdhury P. Kinetic modeling on drug release from controlled drug delivery systems. Acta Pol Pharm. 2010;67(3):217-23. [PMID: 20524422]
- Lokhandwala H, Deshpande A, Deshpande SH. Kinetic modeling and dissolution profiles comparison: an overview. Int J Pharm Bio Sci 2013;4(1):728-3.
- Paarakh MP, Jose PA, Setty CM, Peterchristoper GV. Release kinetics–concepts and applications. Int J Pharm Res Technol 2018;8(1):12-20. [DOI: 10.31838/ijprt/08.01.02]
- Al-Abduljabbar A, Farooq I. Electrospun polymer nanofibers: processing, properties, and applications. Polymers 2022;15(1):65. [DOI: 10.3390/polym15010065]
- Sirin S, Cetiner S, Sarac AS. Polymer nanofibers via electrospinning: factors affecting nanofiber quality. KSU J Eng Sci 2013;16(2):1-12.
- Repanas A, Andriopoulou S, Glasmacher B. The significance of electrospinning as a method to create fibrous scaffolds for biomedical engineering and drug delivery applications. J Drug Deliv Sci Technol. 2016;31:137-46. [DOI: 10.1016/j.jddst.2015.12.007]
- Behbood L, Moradipour P, Moradi F, Arkan E. Mucoadhesive electrospun nanofibers of chitosan/gelatin containing vancomycin as a delivery system. J Rep Pharm Sci 2017;6(2):150-60.
- Alavarse AC, de Oliveira Silva FW, Colque JT, da Silva VM, Prieto T, et al. Tetracycline hydrochloride-loaded electrospun nanofibers mats based on PVA and chitosan for wound dressing. Mater Sci Eng C Mater Biol Appl 2017;77:271-81. [PMID: 28532030 DOI: 10.1016/j.msec.2017.03.199]
- Xia L, Lu L, Liang Y, Cheng B. Fabrication of centrifugally spun prepared poly (lactic acid)/gelatin/ciprofloxacin nanofibers for antimicrobial wound dressing. RSC Adv 2019;9(61):35328-35. [DOI: 10.1039/c9ra07826f]
- Lian H, Meng Z. Melt electrospinning vs. solution electrospinning: a comparative study of drug-loaded poly (ε-caprolactone) fibres. Mater Sci Eng C 2017;74:117-23. [DOI: 10.1016/j.msec.2017.02.024]
- Souza MA, Sakamoto KY, Mattoso LH. Release of the diclofenac sodium by nanofibers of poly (3-hydroxybutyrate-co-3-hydroxyvalerate) obtained from electrospinning and solution blow spinning. J Nanomater 2014;2014:56. [DOI: 10.1155/2014/129035]
- Brako F, Raimi-Abraham BT, Mahalingam S, Craig DQ, Edirisinghe M. The development of progesterone-loaded nanofibers using pressurized gyration: A novel approach to vaginal delivery for the prevention of pre-term birth. Int J Pharm 2018;540(1-2):31-9. [DOI: 10.1016/j.ijpharm.2018.01.043]
- Ding Y, Dou C, Chang S, Xie Z, Yu DG, Liu Y, Shao J. Core–shell eudragit S100 nanofibers prepared via triaxial electrospinning to provide a colon-targeted extended drug release. Polymers (Basel) 2020;12(9):2034. [PMID: 32906728 DOI: 10.3390/polym12092034]
- Yousefi P, Dini G, Movahedi B, Vaezifar S, Mehdikhani M. Polycaprolactone/chitosan core/shell nanofibrous mat fabricated by electrospinning process as carrier for rosuvastatin drug. Polym Bull 2022;79:1627-45. [DOI: 10.1007/s00289-021-03566-4]
- Aras C, Tümay Özer E, Göktalay G, Saat G, Karaca E. Evaluation of Nigella sativa oil loaded electrospun polyurethane nanofibrous mat as wound dressing. J Biomater Sci Polym Ed 2021;32(13):1718-35. [DOI: 10.1080/09205063.2021.1937463]
- Uhljar LÉ, Kan SY, Radacsi N, Koutsos V, Szabó-Révész P, et al. In vitro drug release, permeability, and structural test of ciprofloxacin-loaded nanofibers. Pharmaceutics 2021;13(4):556. [DOI: 10.3390/pharmaceutics13040556]
- Turanlı Y, Tort S, Acartürk F. Development and characterization of methylprednisolone loaded delayed release nanofibers. Int J Drug Deliv Technol 2019;49:58-65. [DOI: 10.1016/j.jddst.2018.10.031]
- Wsoo MA, Abd Razak SI, Bohari SP, Shahir S, Salihu R, et al. Vitamin D3-loaded electrospun cellulose acetate/polycaprolactone nanofibers: characterization, in-vitro drug release and cytotoxicity studies. Int J Biol Macromol 2021;181:82-98. [DOI: 10.1016/j.ijbiomac.2021.03.108]
- Wang Y, Wang B, Qiao W, Yin T. A novel controlled release drug delivery system for multiple drugs based on electrospun nanofibers containing nanoparticles. J Pharm Sci 2010;99(12):4805-11. [PMID: 20821381 DOI: 10.1002/jps.22189]
- Huo P, Han X, Zhang W, Zhang J, Kumar P, et al. Electrospun nanofibers of polycaprolactone/collagen as a sustained-release drug delivery system for artemisinin. Pharmaceutics 2021;13(8):1228. [PMID: 34452189 DOI: 10.3390/pharmaceutics13081228]
- Celebioglu A, Uyar T. Electrospun formulation of acyclovir/cyclodextrin nanofibers for fast-dissolving antiviral drug delivery. Mater Sci Eng C Mater Biol Appl 2021;118:111514. [PMID: 33255070 DOI: 10.1016/j.msec.2020.111514]
- Nguyen VQ, Ishihara M, Kinoda J, Hattori H, Nakamura S, et al. Development of antimicrobial biomaterials produced from chitin-nanofiber sheet/silver nanoparticle composites. J Nanobiotechnology 2014;12:1-9. [PMID: 25467525 DOI: 10.1186/s12951-014-0049-1]
- Darbasizadeh B, Motasadizadeh H, Foroughi-Nia B, Farhadnejad H. Tripolyphosphate-crosslinked chitosan/poly (ethylene oxide) electrospun nanofibrous mats as a floating gastro-retentive delivery system for ranitidine hydrochloride. J Pharm Biomed Anal 2018;153:63-75. [DOI: 10.1016/j.jpba.2018.02.023]
- Irani M, Sadeghi GM, Haririan I. A novel biocompatible drug delivery system of chitosan/temozolomide nanoparticles loaded PCL-PU nanofibers for sustained delivery of temozolomide. Int J Biol Macromol 2017;97:744-51. [PMID: 28109815 DOI: 10.1016/j.ijbiomac.2017.01.073]
- Victor FS, Kugarajah V, Bangaru M, Ranjan S, Dharmalingam S. Electrospun nanofibers of polyvinylidene fluoride incorporated with titanium nanotubes for purifying air with bacterial contamination. Environ Sci Pollut Res 2021;28:37520-33. [DOI: 10.1007/s11356-021-13202-3]
- Yin J, Xu L. Batch preparation of electrospun polycaprolactone/chitosan/aloe vera blended nanofiber membranes for novel wound dressing. Int J Biol Macromol 2020;160:352-63. [DOI: 10.1016/j.ijbiomac.2020.05.211]
- Ahire JJ, Dicks LM. Nisin incorporated with 2, 3-dihydroxybenzoic acid in nanofibers inhibits biofilm formation by a methicillin-resistant strain of staphylococcus aureus. Probiotics Antimicrob Proteins 2015;7:52-9. [PMID: 25319566 DOI: 10.1007/s12602-014-9171-5]
- Gilchrist SE, Lange D, Letchford K, Bach H, Fazli L, et al. Fusidic acid and rifampicin co-loaded PLGA nanofibers for the prevention of orthopedic implant associated infections. J Control Release 2013;170(1):64-73. [DOI: 10.1016/j.jconrel.2013.04.012]
- Sasmal P, Datta P. Tranexamic acid-loaded chitosan electrospun nanofibers as drug delivery system for hemorrhage control applications. Int J Drug Deliv Technol 2019;52:559-67. [DOI: 10.1016/j.jddst.2019.05.018]
- Karthikeyan K, Guhathakarta S, Rajaram R, Korrapati PS. Electrospun zein/eudragit nanofibers based dual drug delivery system for the simultaneous delivery of aceclofenac and pantoprazole. Int J Pharm 2012;438(1-2):117-22. [PMID: 22960320 DOI: 10.1016/j.ijpharm.2012.07.075]
- Hadjianfar M, Semnani D, Varshosaz J. Polycaprolactone/chitosan blend nanofibers loaded by 5-fluorouracil: an approach to anticancer drug delivery system. Polym Adv Technol 2018;29(12):2972-81. [DOI: 10.1002/pat.4417]
- Rahmani F, Ziyadi H, Baghali M, Luo H, Ramakrishna S. Electrospun PVP/PVA nanofiber mat as a novel potential transdermal drug-delivery system for buprenorphine: a solution needed for pain management. Appl Sci 2021;11(6):2779. [DOI: 10.3390/app11062779]
- Mirzaeei S, Mansurian M, Asare-Addo K, Nokhodchi A. Metronidazole-and amoxicillin-loaded PLGA and PCL nanofibers as potential drug delivery systems for the treatment of periodontitis: in vitro and in vivo evaluations. Biomedicines 2021;9(8):975. [PMID: 34440179 DOI: 10.3390/biomedicines9080975]
- Yan E, Jiang J, Yang X, Fan L, Wang Y, et al. pH-sensitive core-shell electrospun nanofibers based on polyvinyl alcohol/polycaprolactone as a potential drug delivery system for the chemotherapy against cervical cancer. Int J Drug Deliv Technol 2020;55:101455. [DOI: 10.1016/j.jddst.2019.101455]
- Wu J, Qin Z, Jiang X, Fang D, Lu Z, Zheng L, Zhao J. ROS-responsive PPGF nanofiber membrane as a drug delivery system for long-term drug release in attenuation of osteoarthritis. NPJ Regen Med 2022;7(1):66. [PMID: 36323709 DOI: 10.1038/s41536-022-00254-3]
- Turanlı Y, Acartürk F. Fabrication and characterization of budesonide loaded colon-specific nanofiber drug delivery systems using anionic and cationic polymethacrylate polymers. Int J Drug Deliv Technol 2021;63:102511. [DOI: 10.1016/j.jddst.2021.102511]
- Brimo N, Uyar T, Uysal B, Dikmen M, Canturk Z. Novel electrospun polymeric nanofibers loaded different medicaments as drug delivery systems for regenerative endodontics. Curr Drug Deliv 2023;20(7):992-1014. [PMID: 35440306 DOI: 10.2174/1567201819666220418102732]
- Paskiabi FA, Bonakdar S, Shokrgozar MA, Imani M, Jahanshiri Z, et al. Terbinafine-loaded wound dressing for chronic superficial fungal infections. Mater Sci Eng C Mater Biol Appl 2017;73:130-6. [PMID: 28183589 DOI: 10.1016/j.msec.2016.12.078]
- Grooms TN, Vuong HR, Tyo KM, Malik DA, Sims LB, et al. Griffithsin-modified electrospun fibers as a delivery scaffold to prevent HIV infection. Antimicrob Agents Chemother 2016;60(11):6518-31. [PMID: 27550363 DOI: 10.1128/AAC.00956-16]
- Davani F, Alishahi M, Sabzi M, Khorram M, Arastehfar A, et al. Dual drug delivery of vancomycin and Imipenem/Cilastatin by coaxial nanofibers for treatment of diabetic foot ulcer infections. Mater Sci Eng C Mater Biol Appl 2021;123:111975. [PMID: 33812603 DOI: 10.1016/j.msec.2021.111975]
- Jani RK, Pate NN, Patel DJ. Nanodispersion loaded nanofibers formulation for the treatment of vulvo-vaginal candidiasis. Indian Patent Application No.: IN202221071107. 2022. [30 Dec 2022]
- Guntaka PCR, Mohan MR, Swapna S, Shaheda S, Bhavanam PR, et al. Preparation and evaluation of drug loaded nanofibers. Indian Patent Application No.: IN202341004551. 2023. [17 Feb 2023]
- Bodas K, Pawar A, Shinde V. Glycyrrhizin loaded nanofiber topical drug delivery for management of chronic wounds. Indian Patent Application No.: IN202321003119. 2023. [27 Jan 2023]
- Gaikwad DT, Shinde KS, Sharma KKK. Construction of Curcumin-Bael fruit gum electrospun nanofibers. Indian Patent Application No.: IN202221030754. 2022. [10 Jun 2022]
- Morad H, Enayatifard R, Jahanshahi M, Akbari J, Saeedi M, et al. International Patent Application No.: WO2020208619. 2020. [15 Oct 2020]
- Stupp SI, Kibbe MR, Karver MR, Peters EB, So M, et al. Drug delivery vehicles for atherosclerosis nanomedicine. U.S. Patent Application No.: US20200289416. 2020. [17 Sep 2020]
- Azzazy HMES, Sarhan WAA. Bio-compatible apitherapeutic nanofiber. International Patent Application No.: WO2015003155. 2016. [8 Jan 2015]
- Becker M, Yu J. Hyperbranched amino acid-based poly(ester urea)s for regenerative medicine and drug deliver. U.S. Patent Application No.: US20160130390. 2017. [19 Aug 2017]
- Zhihong Z, Duanyun C. Double-drug-loading electrostatic spinning nanofiber scaffold as well as preparation method and application there. China Patent Application No.: CN115607527. 2022. [17 Jan 2023]
- Coady DJ, Dipietro RA, Engler AC, Hedrick JL, Liu SQ, et al. Self-assembling bis-urea compounds for drug delivery. U.S. Patent Application No.: US20150037390. 2015. [21 Jul 2015]
- Yliperttula M, Laurén P, Bhattacharya M, Lou Y, Laukkanen A. Drug delivery compositions. European Patent Application No.: EP2632493. 2013. [4 Sep 2013]
- Laurencin CT, Nair LS, Bhattacharyya S, Allcock HR, Bender JD, et al. Polymeric nanofibers for tissue engineering and drug delivery. International Patent Application No.: WO2005025630. 2007. [24 Mar 2005]
- Woodrow K, Ball C, Blakney A, Krogstad E, Nie H. Vaginal matrices: nanofibers for contraception and prevention of HIV infection. U.S. Patent Application No.: US20140128345A1. 2019. [19 Jul 2019]
- Yadong T, Yurong L, Xingzi L, Yaqi W, Feng T, et al. Drug-loaded polydopamine coated nanofiber dressing and preparation method thereof. China Patent Application No.: CN114000262. 2022. [01 Feb 2022]
- Ahmed S. Antimicrobial effect of modified antibiotic nanofibers for regenerative endodontics procedures. Available from: https://clinicaltrials.gov/study/NCT03690960. [Last accessed on 6 Jun 2024]
- Foroughi F. Investigating the efficacy of insert nanofibers containing Vancomycin and Amikacin in patients with infectious keratitis: a phase I randomized clinical trial (RCT) study. Available from: https://irct.behdasht.gov.ir/trial/75765. [Last accessed on 6 Jun 2024]
- Tahvilian R. Synthesis and evaluation of the effect of F. vulgaris nanofibers on burn wounds. Available from: https://irct.behdasht.gov.ir/trial/71282. [Last accessed on 6 Jun 2024]
- Shiva A. Effect of Colchicine on aphthous ulceration. Available from: https://irct.behdasht.gov.ir/trial/66858. [Last accessed on 6 Jun 2024]
- He X. Clinical study of a new liposome nanofibers patch for transdermal drug delivery containing ebracteolata Hayata in the treatment of actinic keratosis. Available from: https://www.chictr.org.cn/showproj.aspx?proj=60090. [Last accessed on 6 Jun 2024]
- Xing L. Clinical study of functional electrospun nanofibers capturing circulating tumor cells from patients with ovarian cancer to predict the efficacy and prognosis of patients with ovarian cancer. Available from: https://www.chictr.org.cn/showproj.aspx?proj=60521. [Last accessed on 6 Jun 2024]
- Zhu H. SVF combined with functional self-assembling peptide nanofiber hydrogels in the treatment of spinal cord injury. Available from: https://clinicaltrials.gov/study/NCT05967325. [Last accessed on 6 Jun 2024]
- Mohamed Hamdy HE-S. Novel silk fibroin nanofiber membrane using minimally invasive surgery in treatment of periodontal intrabony defects: a randomized clinical trial. Available from: https://clinicaltrials.gov/study/NCT06371027. [Last accessed on 6 Jun 2024]